 )
) 1深圳大学心理学院, 深圳 518060
2华中科技大学协和深圳医院, 深圳 518052
3深圳英智科技有限公司, 深圳 518010
收稿日期:2020-08-02出版日期:2021-05-25发布日期:2021-03-29通讯作者:张丹丹E-mail:zhangdd05@gmail.com基金资助:*国家自然科学基金面上项目(31970980);国家自然科学基金面上项目(31871115);深圳市基础研究(自由探索)(JCYJ20180305124305294);深港脑科学创新研究院(2019SHIBS0003)The role of ventrolateral prefrontal cortex on emotional regulation of social pain in depressed patients: A TMS study
MO Licheng1, GUO Tianyou1,2, ZHANG Yueyao1, XU Feng3, ZHANG Dandan1( )
) 1School of Psychology, Shenzhen University, Shenzhen 518060, China
2Union Shenzhen Hospital (Nanshan Hospital), Shenzhen 518052, China
3Shenzhen Yingchi Technology Co. Ltd., Shenzhen 518010, China
Received:2020-08-02Online:2021-05-25Published:2021-03-29Contact:ZHANG Dandan E-mail:zhangdd05@gmail.com摘要/Abstract
摘要: 负性人际交往经历和负性社会事件是抑郁症的重要诱导因素, 而社会功能受损是抑郁症患者的重要特征之一, 患者通常表现出对社会疼痛的情绪失调。为了提高抑郁症患者在负性社交情境中或面对负性社会事件时的情绪调节能力, 本研究采用经颅磁刺激技术(transcranial magnetic stimulation, TMS), 考察抑郁症患者在腹外侧前额叶(the ventrolateral prefrontal cortex, VLPFC)被激活后其情绪调节能力的改变。结果表明, 当右侧VLPFC被TMS激活且患者采用认知重评策略调节情绪时, 实验组患者(n = 64)比对照组患者(n = 63)在社会排斥情境下报告了更弱的负性情绪体验, 这说明激活右侧VLPFC可以有效提高患者对社会疼痛的外显性情绪调节能力。本研究是采用TMS提高抑郁症患者情绪调节能力的首次尝试, 实验发现不但支持了VLPFC与认知重评策略的因果关系, 还为临床改善抑郁症等社会功能障碍患者的情绪调节能力提供了明确的神经治疗靶点。后续研究还需探讨多疗程TMS刺激方案、改变社会疼痛的诱发方式、对比左右侧VLPFC的治疗效果、尝试使用其他的情绪调节策略, 进一步验证本研究的结论, 优化TMS治疗方案。
图/表 4
表1本研究两组患者的人口学特征(M ± SD)
| 变量 | 实验组 (n = 64) | 对照组 (n = 63) | 差异检验 |
|---|---|---|---|
| 年龄(岁) | 29.0 ± 2.3 | 28.8 ± 2.7 | t = 0.5, p= 0.593 |
| 性别(女/男) | 34/30 | 33/30 | χ2 = 0.007, p= 0.933 |
| 抑郁 (BDI-II) | 23.3 ± 6.5 | 22.3 ± 5.8 | t = 0.9, p= 0.382 |
| 社交焦虑(LSAS) | 39.4 ± 20.2 | 39.8 ± 20.3 | t = -0.1, p= 0.911 |
| 拒绝敏感性(RSQ) | 9.0 ± 3.4 | 8.8 ± 3.8 | t = 0.3, p= 0.763 |
| 共情(IRI) | 51.1 ± 9.7 | 49.4 ± 10.5 | t = 1.0, p= 0.328 |
表1本研究两组患者的人口学特征(M ± SD)
| 变量 | 实验组 (n = 64) | 对照组 (n = 63) | 差异检验 |
|---|---|---|---|
| 年龄(岁) | 29.0 ± 2.3 | 28.8 ± 2.7 | t = 0.5, p= 0.593 |
| 性别(女/男) | 34/30 | 33/30 | χ2 = 0.007, p= 0.933 |
| 抑郁 (BDI-II) | 23.3 ± 6.5 | 22.3 ± 5.8 | t = 0.9, p= 0.382 |
| 社交焦虑(LSAS) | 39.4 ± 20.2 | 39.8 ± 20.3 | t = -0.1, p= 0.911 |
| 拒绝敏感性(RSQ) | 9.0 ± 3.4 | 8.8 ± 3.8 | t = 0.3, p= 0.763 |
| 共情(IRI) | 51.1 ± 9.7 | 49.4 ± 10.5 | t = 1.0, p= 0.328 |

图1实验材料及实验流程。A, 实验材料示例。本实验部分图片选自互联网, 为了不侵犯他人版权和肖像权, 此处图片中的人物为课题组研究生。B, 单个试次的刺激呈现内容。C, 实验流程图。
 图1实验材料及实验流程。A, 实验材料示例。本实验部分图片选自互联网, 为了不侵犯他人版权和肖像权, 此处图片中的人物为课题组研究生。B, 单个试次的刺激呈现内容。C, 实验流程图。
图1实验材料及实验流程。A, 实验材料示例。本实验部分图片选自互联网, 为了不侵犯他人版权和肖像权, 此处图片中的人物为课题组研究生。B, 单个试次的刺激呈现内容。C, 实验流程图。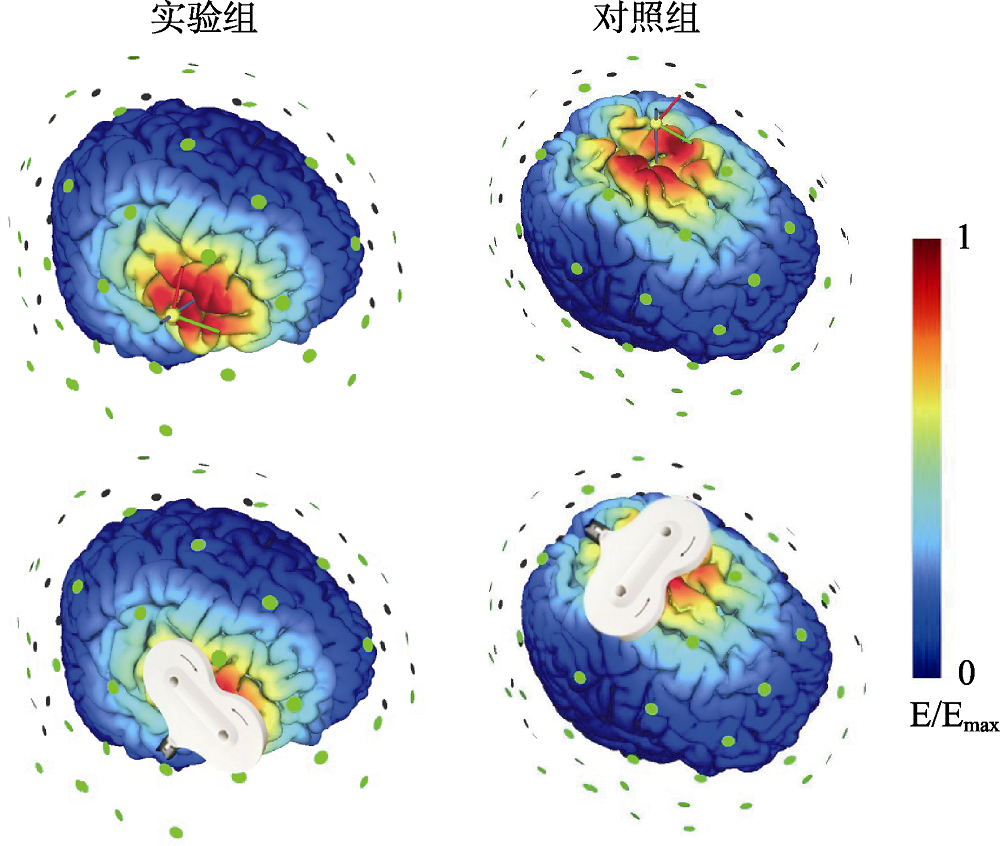
图2TMS电流分布模拟图。图中的颜色代表了归一化的电流场强度, 蓝色表示0, 红色表示个体最大值。
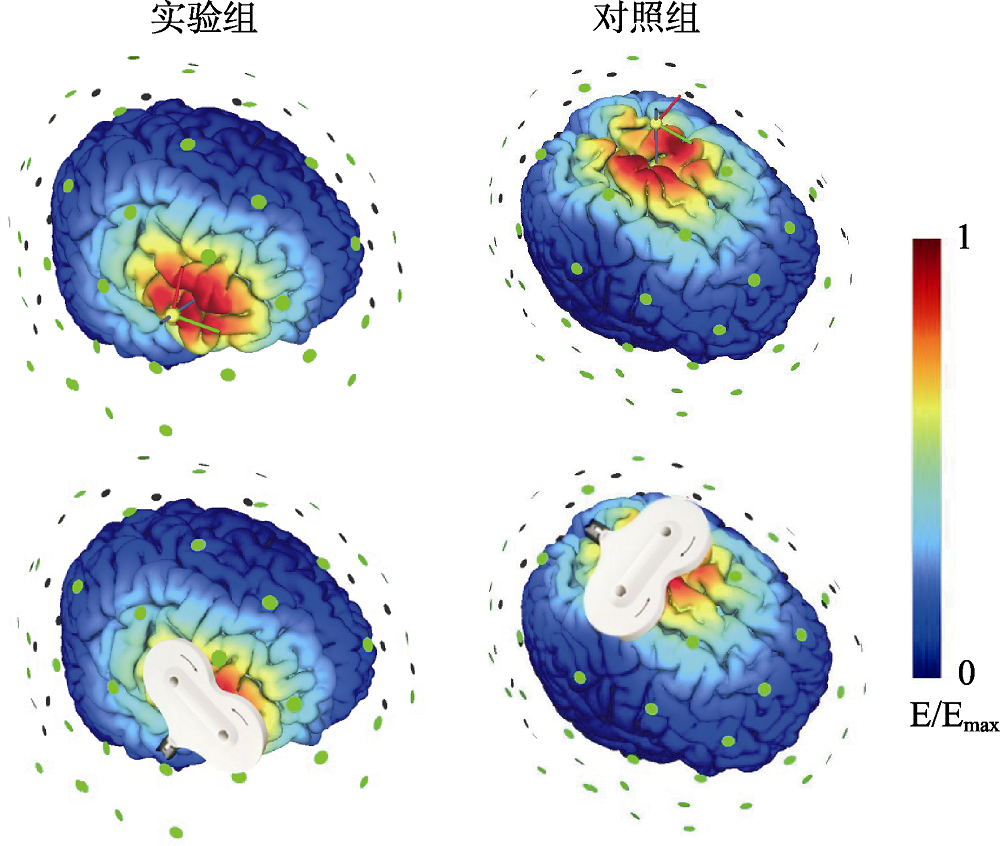 图2TMS电流分布模拟图。图中的颜色代表了归一化的电流场强度, 蓝色表示0, 红色表示个体最大值。
图2TMS电流分布模拟图。图中的颜色代表了归一化的电流场强度, 蓝色表示0, 红色表示个体最大值。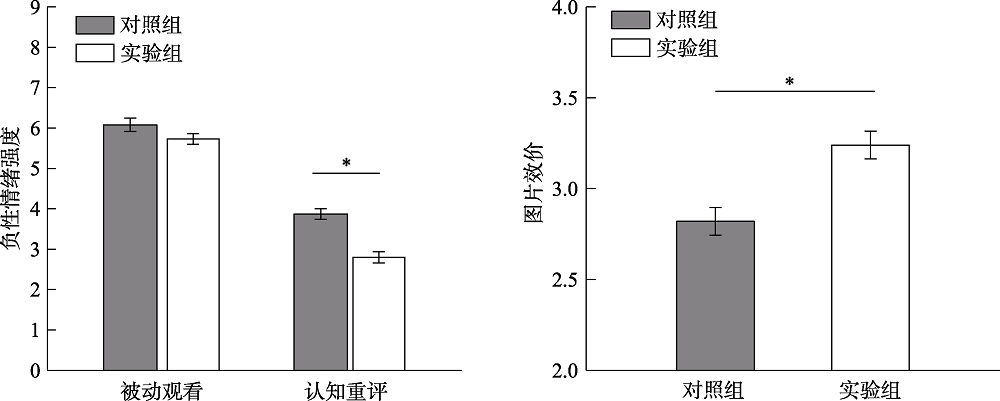
图3实验结果。A, 被动观看和认知重评过程中的负性情绪强度评分(1~9点评分, 1分表示最低强度的负性情绪, 9分表示最高强度的负性情绪)。B, 情绪调节30 min后的图片效价评分(1~9点评分, 1分表示最负性, 9分表示最正性)。图中的误差条表示均值的标准误。*p < 0.05。
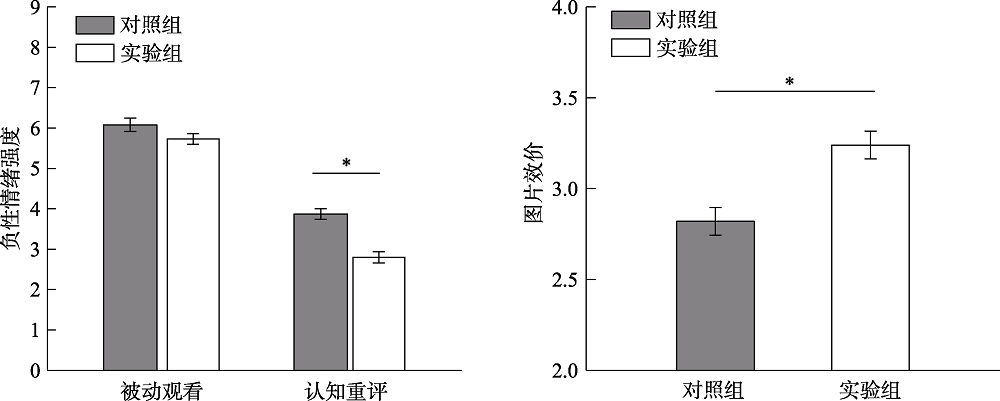 图3实验结果。A, 被动观看和认知重评过程中的负性情绪强度评分(1~9点评分, 1分表示最低强度的负性情绪, 9分表示最高强度的负性情绪)。B, 情绪调节30 min后的图片效价评分(1~9点评分, 1分表示最负性, 9分表示最正性)。图中的误差条表示均值的标准误。*p < 0.05。
图3实验结果。A, 被动观看和认知重评过程中的负性情绪强度评分(1~9点评分, 1分表示最低强度的负性情绪, 9分表示最高强度的负性情绪)。B, 情绪调节30 min后的图片效价评分(1~9点评分, 1分表示最负性, 9分表示最正性)。图中的误差条表示均值的标准误。*p < 0.05。 参考文献 100
| [1] | Ajaya, Y., Peckham, A. D., & Johnson, S.L. (2016). Emotion regulation and mania risk: Differential responses to implicit and explicit cues to regulate. Journal of Behavior Therapy and Experimental Psychiatry, 50,283-288. |
| [2] | Allen, J.J. B., & Reznik, S.J. (2015). Frontal EEG asymmetry as a promising marker of depression vulnerability: Summary and methodological considerations. Current Opinion in Psychology, 4,93-97. doi: 10.1016/j.copsyc.2014.12.017URLpmid: 26462291 |
| [3] | APA. APA. (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th ed. American Psychiatric Association, Washington, DC. |
| [4] | Beck, A. T., & Alford, B.A. (2009). Depression: Causes and Treatment (2nd Edition). Philadelphia, Pennsylvania: University of Pennsylvania Press, Inc. |
| [5] | Beck, A.T., Steer, R. A., & Brown, G.K. (1996). Beck Depression Inventory-Second Edition Manual. San Antonio, TX: The Psychological Corporation. |
| [6] | Berkman, E. T., & Lieberman, M.D. (2009). Using Neuroscience to Broaden Emotion Regulation: Theoretical and Methodological Considerations. Social and Personality Psychology Compass, 3(4),475-493. doi: 10.1111/j.1751-9004.2009.00186.xURLpmid: 24052803 |
| [7] | Brunoni, A.R., Ferrucci, R., Fregni, F., Boggio, P. S., & Priori, A. (2012). Transcranial direct current stimulation for the treatment of major depressive disorder: A summary of preclinical, clinical and translational findings. Progress in Neuro-psychopharmacology & Biological Psychiatry, 39(1),9-16. doi: 10.1016/j.pnpbp.2012.05.016URLpmid: 22651961 |
| [8] | Buhle, J.T., Silvers, J.A., Wager, T.D., Lopez, R., Onyemekwu, C., Kober, H., Weber, J., & Ochsner, K.N. (2014). Cognitive reappraisal of emotion: A meta-analysis of human neuroimaging studies. Cerebral Cortex, 24(11),2981-2990. |
| [9] | Cavaleri, R., Schabrun, S. M., & Chipchase, L.S. (2017). The number of stimuli required to reliably assess corticomotor excitability and primary motor cortical representations using transcranial magnetic stimulation (TMS): A systematic review and meta-analysis. Systematic Reviews, 6(1),48. doi: 10.1186/s13643-017-0440-8URLpmid: 28264713 |
| [10] | Chester, D.S., Lynam, D.R., Milich, R., & DeWall, C.N. (2018). Neural mechanisms of the rejection-aggression link. Social Cognitive and Affective Neuroscience, 13(5),501-512. doi: 10.1093/scan/nsy025URLpmid: 29618118 |
| [11] | Davey, C.G., Allen, N.B., Harrison, B. J., & Yücel, M. (2011). Increased amygdala response to positive social feedback in young people with major depressive disorder. Biological Psychiatry, 69(8),734-741. |
| [12] | Davis, M.H. (1980). A multidimensional approach to individual differences in empathy. Journal of Personality & Social Psychology, 10,85. |
| [13] | DeWall, C.N., Twenge, J.M., Koole, S.L., Baumeister, R.F., Marquez, A., & Reid, M.W. (2011). Automatic emotion regulation after social exclusion: Tuning to positivity. Emotion, 11(3),623-636. |
| [14] | D?rfel, D., Lamke, J.P., Hummel, F., Wagner, U., Erk, S., & Walter, H. (2014). Common and differential neural networks of emotion regulation by detachment, reinterpretation, distraction, and expressive suppression: A comparative fMRI investigation. NeuroImage, 101,298-309. doi: 10.1016/j.neuroimage.2014.06.051URLpmid: 24993897 |
| [15] | Downar, J., & Daskalakis, Z.J. (2013). New targets for rTMS in depression: A review of convergent evidence. Brain Stimulation, 6(3),231-240. |
| [16] | Downey, G., & Feldman, S.I. (1996). Implications of rejection sensitivity for intimate relationships. Journal of Personality and Social Psychology, 70(6),1327-1343. |
| [17] | Dryman, M. T., & Heimberg, R.G. (2018). Emotion regulation in social anxiety and depression: A systematic review of expressive suppression and cognitive reappraisal. Clinical Psychology Review, 65,17-42. URLpmid: 30064053 |
| [18] | Eisenberger, N.I. (2012). The pain of social disconnection: Examining the shared neural underpinnings of physical and social pain. Nature Reviews Neuroscience, 13(6),421-434. |
| [19] | Eisenberger, N.I. (2015). The pain of social disconnection: Examining the shared neural underpinnings of physical and social pain.e. Annual Review of Psychology, 66,601-629. |
| [20] | Eisenberger, N. I., & Lieberman, M.D. (2004). Why rejection hurts: A common neural alarm system for physical and social pain. Trends in Cognitive Sciences, 8(7),294-300. URLpmid: 15242688 |
| [21] | Eisenberger, N.I., Lieberman, M. D., & Williams, K.D. (2003). Does rejection hurt? An FMRI study of social exclusion. Science, 302(5643),290-292. |
| [22] | Elliott, R., Lythe, K.E., Lee, R., McKie, S., Juhasz, G., Thomas, E.J., … Anderson, I.M. (2012). Reduced medial prefrontal responses to social interaction images in remitted depression. Archives of General Psychiatry, 69(1),37-45. doi: 10.1001/archgenpsychiatry.2011.139URLpmid: 22213787 |
| [23] | Erk, S., Mikschl, A., Stier, S., Ciaramidaro, A., Gapp, V., Weber, B., & Walter, H. (2010). Acute and sustained effects of cognitive emotion regulation in major depression. The Journal of Neuroscience, 30(47),15726-15734. |
| [24] | Etkin, A., Büchel, C., & Gross, J.J. (2015). The neural bases of emotion regulation. Nature Reviews. Neuroscience, 16(11),693-700. doi: 10.1038/nrn4044URLpmid: 26481098 |
| [25] | George, M.S., Lisanby, S.H., Avery, D., McDonald, W.M., Durkalski, V., Pavlicova, M., … Sackeim, H.A. (2010). Daily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: A sham-controlled randomized trial. Archives of General Psychiatry, 67(5),507-516. |
| [26] | Goldin, P.R., McRae, K., Ramel, W., & Gross, J.J. (2008). The neural bases of emotion regulation: Reappraisal and suppression of negative emotion. Biological Psychiatry, 63(6),577-586. |
| [27] | Gotlib, I. H., & Joormann, J. (2010). Cognition and depression: Current status and future directions. Annual Review of Clinical Psychology, 6,285-312. doi: 10.1146/annurev.clinpsy.121208.131305URLpmid: 20192795 |
| [28] | Hamilton, J.P., Etkin, A., Furman, D.J., Lemus, M.G., Johnson, R. F., & Gotlib, I.H. (2012). Functional neuroimaging of major depressive disorder: A meta-analysis and new integration of base line activation and neural response data. The American Journal of Psychiatry, 169(7),693-703. doi: 10.1176/appi.ajp.2012.11071105URLpmid: 22535198 |
| [29] | Hammen, C. (2005). Stress and depression. Annual Review of Clinical Psychology, 1,293-319. doi: 10.1146/annurev.clinpsy.1.102803.143938URLpmid: 17716090 |
| [30] | Hartwright, C.E., Hardwick, R.M., Apperly, I. A., & Hansen, P.C. (2016). Resting state morphology predicts the effect of theta burst stimulation in false belief reasoning. Human Brain Mapping, 37(10),3502-3514. |
| [31] | Helion, C., Krueger, S. M., & Ochsner, K.N. (2019). Emotion regulation across the life span. Handbook of Clinical Neurology, 163,257-280. doi: 10.1016/B978-0-12-804281-6.00014-8URLpmid: 31590734 |
| [32] | Heller, A.S., Johnstone, T., Peterson, M.J., Kolden, G.G., Kalin, N. H., & Davidson, R.J. (2013). Increased prefrontal cortex activity during negative emotion regulation as a predictor of depression symptom severity trajectory over 6 months. JAMA Psychiatry, 70(11),1181-1189. |
| [33] | Henriques, J. B., & Davidson, R.J. (1991). Left frontal hypoactivation in depression. Journal of Abnormal Psychology, 100(4),535-545. |
| [34] | Henriques, J. B., & Davidson, R.J. (2000). Decreased responsiveness to reward in depression. Cognition and Emotion, 14(5),711-724. |
| [35] | Herbsman, T., Avery, D., Ramsey, D., Holtzheimer, P., Wadjik, C., Hardaway, F.,… Nahas, Z. (2009). More lateral and anterior prefrontal coil location is associated with better repetitive transcranial magnetic stimulation antidepressant response. Biological Psychiatry, 66(5),509-515. |
| [36] | He, Z., Lin, Y., Xia, L., Liu, Z., Zhang, D., & Elliott, R. (2018). Critical role of the right VLPFC in emotional regulation of social exclusion: A tDCS study. Social Cognitive and Affective Neuroscience, 13(4),357-366. URLpmid: 29618116 |
| [37] | He, Z., Liu, Z., Zhao, J., Elliott, R., & Zhang, D. (2019). Improving emotion regulation of social exclusion in depression-prone individuals: A tDCS study targeting right VLPFC. Psychological Medicine, doi: 10.1017/S0033291719002915.Online ahead of print. URLpmid: 33875023 |
| [38] | He, Z., Zhao, J., Shen, J., Muhlert, N., Elliott, R., & Zhang, D. (2020). The right VLPFC and downregulation of social pain: A TMS study. Human Brain Mapping, 41(5),1362-1371. URLpmid: 31789480 |
| [39] | Hooker, C.I., Gyurak, A., Verosky, S.C., Miyakawa, A., & Ayduk, O. (2010). Neural activity to a partner's facial expression predicts self-regulation after conflict. Biological Psychiatry, 67(5),406-413. |
| [40] | Horvath, J.C., Forte, J.D., Carter, O. (2015). Quantitative review finds no evidence of cognitive effects in healthy populations from single-session transcranial direct current stimulation (tDCS). Brain Stimulation, 8(3),535-550. |
| [41] | Hsu, D.T., Sanford, B.J., Meyers, K.K., Love, T.M., Hazlett, K.E., Walker, S.J., … Zubieta, J.-K. (2015). It still hurts: Altered endogenous opioid activity in the brain during social rejection and acceptance in major depressive disorder. Molecular Psychiatry, 20(2),193-200. doi: 10.1038/mp.2014.185URLpmid: 25600108 |
| [42] | Jankowski, K.F., Batres, J., Scott, H., Smyda, G., Pfeifer, J. H., & Quevedo, K. (2018). Feeling left out: Depressed adolescents may atypically recruit emotional salience and regulation networks during social exclusion. Social Cognitive and Affective Neuroscience, 13(8),863-876. URLpmid: 30059994 |
| [43] | Koban, L., Jepma, M., Geuter, S., & Wager, T.D. (2017). What's in a word? How instructions, suggestions, and social information change pain and emotion. Neuroscience and Biobehavioral Reviews, 81(Pt A),29-42. doi: 10.1016/j.neubiorev.2017.02.014URLpmid: 29173508 |
| [44] | Kohn, N., Eickhoff, S.B., Scheller, M., Laird, A. R., Fox, P. T., & Habel, U. (2014). Neural network of cognitive emotion regulation -- An ALE meta-analysis and MACM analysis. NeuroImage, 87,345-355. |
| [45] | Kupferberg, A., Bicks, L., & Hasler, G. (2016). Social functioning in major depressive disorder. Neuroscience and Biobehavioral Reviews, 69,313-332. |
| [46] | Laceulle, O.M., Veenstra, R., Vollebergh, W.A. M., & Ormel, J. (2019). Sequences of maladaptation: Preadolescent self-regulation, adolescent negative social interactions, and young adult psychopathology. Development and Psychopathology, 31(1),279-292. URLpmid: 29229016 |
| [47] | Lau, J.Y. F., & Waters, A.M. (2017). Annual research review: An expanded account of information-processing mechanisms in risk for child and adolescent anxiety and depression. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 58(4),387-407. doi: 10.1111/jcpp.12653URLpmid: 27966780 |
| [48] | Lieberman, M.D., Inagaki, T.K., Tabibnia, G., & Crockett, M.J. (2011). Subjective responses to emotional stimuli during labeling, reappraisal, and distraction. Emotion, 11(3),468-480. |
| [49] | Lieberman, M.D., Jarcho, J.M., Berman, S., Naliboff, B.D., Suyenobu, B.Y., Mandelkern, M., & Mayer, E.A. (2004). The neural correlates of placebo effects: A disruption account. Neuroimage, 22(1),447-455. |
| [50] | Liebowitz, M.R. (1987). Social phobia. Modern Problems in Pharmacopsychiatry, 22,141-173. |
| [51] | MacDonald, G., Kingsury, R., & Shaw, S. (2005). Adding insult to injury:Social pain theory and response to social exclusion. In K. D. Williams, J. P. Forgas, & W. von Hippel. (Eds.), Forgas ,Sydney symposium of social psychology series the social outcast: Ostracism, social exclusion, rejection, & bullying (pp.77-90). New York: Psychology Press. |
| [52] | Marques, L.M., Morello, L.Y. N., & Boggio, P.S. (2018). Ventrolateral but not dorsolateral prefrontal cortex tDCS effectively impact emotion reappraisal-effects on emotional experience and interbeat interval. Scientific Reports, 8(1),15295. doi: 10.1038/s41598-018-33711-5URLpmid: 30333566 |
| [53] | Masina, F., Tarantino, V., Vallesi, A., & Mapelli, D. (2019). Repetitive TMS over the left dorsolateral prefrontal cortex modulates the error positivity: An ERP study. Neuropsychologia, 133,107153. doi: 10.1016/j.neuropsychologia.2019.107153URLpmid: 31398426 |
| [54] | Masten, C.L., Eisenberger, N.I., Borofsky, L.A., Pfeifer, J.H., McNealy, K., Mazziotta, J. C., & Dapretto, M. (2009). Neural correlates of social exclusion during adolescence: Understanding the distress of peer rejection. Social Cognitive and Affective Neuroscience, 4(2),143-157. |
| [55] | Moodie, C.A., Suri, G., Goerlitz, D.S., Mateen, M.A., Sheppes, G., McRae, K., … Gross, J.J. (2020). The neural bases of cognitive emotion regulation: The roles of strategy and intensity. Cognitive, Affective & Behavioral Neuroscience, 20(2),387-407. doi: 10.3758/s13415-020-00775-8URLpmid: 32133586 |
| [56] | Morawetz, C., Bode, S., Baudewig, J., Kirilina, E., & Heekeren, H.R. (2016). Changes in effective connectivity between dorsal and ventral prefrontal regions moderate emotion regulation. Cerebral Cortex, 26(5),1923-1937. doi: 10.1093/cercor/bhv005URLpmid: 25631055 |
| [57] | Morawetz, C., Bode, S., Derntl, B., & Heekeren, H.R. (2017). The effect of strategies, goals and stimulus material on the neural mechanisms of emotion regulation: A meta-analysis of fMRI studies. Neuroscience and Biobehavioral Reviews, 72,111-128. doi: 10.1016/j.neubiorev.2016.11.014URLpmid: 27894828 |
| [58] | Nolan, S.A., Flynn, C., & Garber, J. (2003). Prospective relations between rejection and depression in young adolescents. Journal of Personality and Social Psychology, 85(4),745-755. |
| [59] | Ochsner, K.N., Bunge, S.A., Gross, J. J., & Gabrieli, J.D. E. (2002). Rethinking feelings: An FMRI study of the cognitive regulation of emotion. Journal of Cognitive Neuroscience, 14(8),1215-1229. |
| [60] | Ochsner, K.N., Ray, R.D., Cooper, J.C., Robertson, E.R., Chopra, S., Gabrieli, J.D. E., & Gross, J.J. (2004). For better or for worse: Neural systems supporting the cognitive down- and up-regulation of negative emotion. NeuroImage, 23(2),483-499. |
| [61] | Ochsner, K.N., Silvers, J. A., & Buhle, J.T. (2012). Functional imaging studies of emotion regulation:A synthetic review and evolving model of the cognitive control of emotion. Annals of the New York Academy of Sciences, 1251,E1-24. |
| [62] | Onoda, K., Okamoto, Y., Nakashima, K.'i., Nittono, H., Yoshimura, S., Yamawaki, S., … Ura, M. (2010). Does low self-esteem enhance social pain? The relationship between trait self-esteem and anterior cingulate cortex activation induced by ostracism. Social Cognitive and Affective Neuroscience, 5(4),385-391. |
| [63] | Paillere Martinot M.-L., Martinot, J.-L., Ringuenet, D., Galinowski, A., Gallarda, T., Bellivier, F., … Eric A. (2011). Baseline brain metabolism in resistant depression and response to transcranial magnetic stimulation. Neuropsychopharmacology, 36(13),2710e9. |
| [64] | Park, C., Rosenblat, J.D., Lee, Y., Pan, Z., Cao, B., Iacobucci, M., & McIntyre, R.S. (2019). The neural systems of emotion regulation and abnormalities in major depressive disorder. Behavioural Brain Research, 367,181-188. doi: 10.1016/j.bbr.2019.04.002URLpmid: 30951753 |
| [65] | Paul, S., Simon, D., Kniesche, R., Kathmann, N., & Endrass, T. (2013). Timing effects of antecedent- and response-focused emotion regulation strategies. Biological Psychology, 94(1),136-142. |
| [66] | Pfabigan, D.M., Alexopoulos, J., Bauer, H., & Sailer, U. (2011). Manipulation of feedback expectancy and valence induces negative and positive reward prediction error signals manifest in event-related brain potentials. Psychophysiology, 48(5),656-664. |
| [67] | Phillips, M.L., Ladouceur, C. D., & Drevets, W.C. (2008). A neural model of voluntary and automatic emotion regulation: Implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Molecular Psychiatry, 13(9),829-857. |
| [68] | Picó-Pérez, M., Radua, J., Steward, T., Menchón, J. M., & Soriano-Mas, C. (2017). Emotion regulation in mood and anxiety disorders: A meta-analysis of fMRI cognitive reappraisal studies. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 79(Pt B),96-104. URLpmid: 28579400 |
| [69] | Pitskel, N.B., Bolling, D.Z., Kaiser, M.D., Pelphrey, K. A., & Crowley, M.J. (2014). Neural systems for cognitive reappraisal in children and adolescents with autism spectrum disorder. Developmental Cognitive Neuroscience, 10,117-128. |
| [70] | Price, A. R., & Hamilton, R.H. (2015). A re-evaluation of the cognitive effects from single-session transcranial direct current stimulation. Brain Stimulation, 8(3),663-665. |
| [71] | Price, R.B., Paul, B., Schneider, W., & Siegle, G.J. (2013). Neural correlates of three neurocognitive intervention strategies: A preliminary step towards personalized treatment for psychological disorders. Cognitive Therapy and Research, 37(4),657-672. doi: 10.1007/s10608-012-9508-xURLpmid: 23935231 |
| [72] | Riva, P., & Eck, J. (2016). Social exclusion: Psychological approaches to understanding and reducing its impact. New York: Springer. |
| [73] | Riva, P., Romero Lauro, L.J., DeWall, C. N., & Bushman, B.J. (2012). Buffer the pain away: Stimulating the right ventrolateral prefrontal cortex reduces pain following social exclusion. Psychological Science, 23(12),1473-1475. |
| [74] | Riva, P., Romero Lauro, L.J., DeWall, C.N., Chester, D. S., & Bushman, B.J. (2015). Reducing aggressive responses to social exclusion using transcranial direct current stimulation. Social Cognitive and Affective Neuroscience, 10(3),352-356. |
| [75] | Riva, P., Romero Lauro, L.J., Vergallito, A., DeWall, C. N., & Bushman, B.J. (2015). Electrified emotions: Modulatory effects of transcranial direct stimulation on negative emotional reactions to social exclusion. Social Neuroscience, 10(1),46-54. doi: 10.1080/17470919.2014.946621URLpmid: 25139575 |
| [76] | Rive, M.M., van Rooijen, G., Veltman, D.J., Phillips, M.L., Schene, A. H., & Ruhé, H.G. (2013). Neural correlates of dysfunctional emotion regulation in major depressive disorder. A systematic review of neuroimaging studies. Neuroscience and Biobehavioral Reviews, 37(10 Pt 2), 2529-2553. doi: 10.1016/j.neubiorev.2012.11.001URL |
| [77] | Scarpa, A., & Reyes, N.M. (2011). Improving emotion regulation with CBT in young children with high functioning autism spectrum disorders: A pilot study. Behavioural and Cognitive Psychotherapy, 39(4),495-500. doi: 10.1017/S1352465811000063URLpmid: 21457605 |
| [78] | Sch?fer, J.?., Naumann, E., Holmes, E.A., Tuschen-Caffier, B., & Samson, A.C. (2017). Emotion regulation strategies in depressive and anxiety symptoms in youth: A meta-analytic review. Journal of Youth and Adolescence, 46(2),261-276. doi: 10.1007/s10964-016-0585-0URLpmid: 27734198 |
| [79] | Schmaal, L., van Harmelen, A.-L., Chatzi, V., Lippard, E.T. C., Toenders, Y.J., Averill, L.A., … Blumberg, H.P. (2020). Imaging suicidal thoughts and behaviors: A comprehensive review of 2 decades of neuroimaging studies. Molecular Psychiatry, 25(2),408-427. doi: 10.1038/s41380-019-0587-xURLpmid: 31787757 |
| [80] | Schutter, D.J. (2010). Quantitative review of the efficacy of slow-frequency magnetic brain stimulation in major depressive disorder. Psychological Medicine, 40(11),1789-1795. |
| [81] | Sebastian, C.L., Tan, G.C.Y., Roiser, J.P., Viding, E., Dumontheil, I., & Blakemore, S.J. (2011). Developmental influences on the neural bases of responses to social rejection: Implications of social neuroscience for education. NeuroImage, 57(3),686-694. |
| [82] | Silvers, J.A., Insel, C., Powers, A., Franz, P., Helion, C., Martin, R.E., … Ochsner, K.N. (2017). Vlpfc-vmPFC- Amygdala interactions underlie age-related differences in cognitive regulation of emotion. Cerebral Cortex, 27(7),3502-3514. doi: 10.1093/cercor/bhw073URLpmid: 27341851 |
| [83] | Smith, K. (2014). Mental health: A world of depression. Nature, 515(7526),181. URLpmid: 25391942 |
| [84] | Smits, F.M., Schutter, D., van Honk, J., & Geuze, E. (2020). Does non-invasive brain stimulation modulate emotional stress reactivity? Social Cognitive and Affective Neuroscience, 15(1),23-51. doi: 10.1093/scan/nsaa011URLpmid: 31993648 |
| [85] | Somani, A., & Kar, S.K. (2019). Efficacy of repetitive transcranial magnetic stimulation in treatment-resistant depression: The evidence thus far. General Psychiatry, 32(4),e100074. URLpmid: 31552384 |
| [86] | Song, S.S., Zilverstand, A., Gui, W. J., Li, H. -J., & Zhou, X.L. (2019). Effects of single-session versus multi-session non-invasive brain stimulation on craving and consumption in individuals with drug addiction, eating disorders or obesity: A meta-analysis. Brain Stimulation, 12(3),606-618. doi: 10.1016/j.brs.2018.12.975URLpmid: 30612944 |
| [87] | Taylor Tavares J.V., Clark, L., Furey, M.L., Williams, G.B., Sahakian B. J., & Drevets, W.C. (2008). Neural basis of abnormal response to negative feedback in unmedicated mood disorders. NeuroImage, 42(3),1118-1126. |
| [88] | Thut, G., & Pascual-Leone, A. (2010). A review of combined TMS-EEG studies to characterize lasting effects of repetitive TMS and assess their usefulness in cognitive and clinical neuroscience. Brain Topography, 22(4),219-232. |
| [89] | Valero-Cabré, A., Amengual, J.L., Stengel, C., Pascual-Leone, A., & Coubard, O.A. (2017). Transcranial magnetic stimulation in basic and clinical neuroscience: A comprehensive review of fundamental principles and novel insights. Neuroscience and Biobehavioral Reviews, 83,381-404. doi: 10.1016/j.neubiorev.2017.10.006URLpmid: 29032089 |
| [90] | Vanneste, S., & de Ridder, D. (2013). Differences between a single session and repeated sessions of 1 Hz TMS by double-cone coil prefrontal stimulation for the improvement of tinnitus. Brain Stimulation, 6(2),155-159. |
| [91] | Vijayakumar, N., Cheng, T. W., & Pfeifer, J.H. (2017). Neural correlates of social exclusion across ages: A coordinate- based meta-analysis of functional MRI studies. NeuroImage, 153,359-368. doi: 10.1016/j.neuroimage.2017.02.050URLpmid: 28235565 |
| [92] | Visted, E., V?llestad, J., Nielsen, M. B., & Schanche, E. (2018). Emotion regulation in current and remitted depression: A systematic review and meta-analysis. Frontiers in Psychology, 9,756. doi: 10.3389/fpsyg.2018.00756URLpmid: 29867700 |
| [93] | Wager, T.D., Davidson, M.L., Hughes, B.L., Lindquist, M. A., & Ochsner, K.N. (2008). Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron, 59(6),1037-1050. |
| [94] | Wang, H., Braun, C., & Enck, P. (2017). How the brain reacts to social stress (exclusion)-A scoping review. Neuroscience and Biobehavioral Reviews, 80,80-88. doi: 10.1016/j.neubiorev.2017.05.012URLpmid: 28535967 |
| [95] | Wiech, K., Ploner, M., & Tracey, I. (2008). Neurocognitive aspects of pain perception. Trends on Cognitive Science, 12(8),306-313. |
| [96] | Yanagisawa, K., Masui, K., Furutani, K., Nomura, M., Ura, M., & Yoshida, H. (2011). Does higher general trust serve as a psychosocial buffer against social pain? An NIRS study of social exclusion. Social Neuroscience, 6(2),190-197. |
| [97] | Yuan, J., Ding, N., Liu, Y., & Yang, J. (2015). Unconscious emotion regulation: Nonconscious reappraisal decreases emotion-related physiological reactivity during frustration. Cognition & Emotion, 29(6),1042-1053. |
| [98] | Zhang, D.D., Liu Z.L., Chen, Y., & Mai, X.Q. (2019). The role of right ventrolateral prefrontal cortex on social emotional regulation in subclinical depression: An tDCS study. Acta Psychologica Sinica, 51(2),207-215. |
| [ 张丹丹, 刘珍莉, 陈钰, 买晓琴. (2019). 右腹外侧前额叶对高抑郁水平成年人社会情绪调节的作用:一项tDCS研究. 心理学报, 51(2),207-215.] | |
| [99] | Zilverstand, A., Parvaz, M. A., & Goldstein, R.Z. (2017). Neuroimaging cognitive reappraisal in clinical populations to define neural targets for enhancing emotion regulation. A systematic review. NeuroImage, 151,105-116. doi: 10.1016/j.neuroimage.2016.06.009URLpmid: 27288319 |
| [100] | Zwanzger, P., Steinberg, C., Rehbein, A.M., Br?ckelmann, A.-K., Dobel, C., Zavorotnyy, M., … Jungh?fer, M. (2014). NeuroImage Inhibitory repetitive transcranial magnetic stimulation (rTMS) of the dorsolateral prefrontal cortex modulates early affective processing. NeuroImage. 101,193-203. doi: 10.1016/j.neuroimage.2014.07.003URLpmid: 25019678 |
相关文章 15
| [1] | 袁加锦, 张祎程, 陈圣栋, 罗利, 茹怡珊. 中国情绪调节词语库的初步编制与试用[J]. 心理学报, 2021, 53(5): 445-455. |
| [2] | 华艳, 李明霞, 王巧婷, 冯彩霞, 张晶. 左侧眶额皮层在自动情绪调节下注意选择中的作用:来自经颅直流电刺激的证据[J]. 心理学报, 2020, 52(9): 1048-1056. |
| [3] | 曹娜,孟海江,王艳秋,邱方晖,谭晓缨,吴殷,张剑. 左侧背外侧前额叶在程序性运动学习中的作用[J]. 心理学报, 2020, 52(5): 597-608. |
| [4] | 孙岩, 吕娇娇, 兰帆, 张丽娜. 自我关注重评和情境关注重评情绪调节策略及对随后认知控制的影响[J]. 心理学报, 2020, 52(12): 1393-1406. |
| [5] | 孙岩,薄思雨,吕娇娇. 认知重评和表达抑制情绪调节策略的脑网络分析:来自EEG和ERP的证据[J]. 心理学报, 2020, 52(1): 12-25. |
| [6] | 孙俊才,寻凤娇,刘萍,张文海. 高善良特质在情绪调节行动控制中的内隐优势[J]. 心理学报, 2019, 51(7): 781-794. |
| [7] | 李红,杨小光,郑文瑜,王超. 抑郁倾向对个体情绪调节目标的影响——来自事件相关电位的证据[J]. 心理学报, 2019, 51(6): 637-647. |
| [8] | 彭婉晴,罗帏,周仁来. 工作记忆刷新训练改善抑郁倾向大学生情绪调节能力的HRV证据[J]. 心理学报, 2019, 51(6): 648-661. |
| [9] | 张丹丹,刘珍莉,陈钰,买晓琴. 右腹外侧前额叶对高抑郁水平成年人社会情绪调节的作用:一项tDCS研究[J]. 心理学报, 2019, 51(2): 207-2015. |
| [10] | 叶婉青, 李晓彤, 王大华. 老年人对夫妻间负性事件的认知性情绪调节策略及其与婚姻满意度的关系:交叉滞后分析[J]. 心理学报, 2018, 50(4): 426-435. |
| [11] | 吕梦思, 席居哲, 罗一睿. 不同心理弹性者的日常情绪特征: 结合体验采样研究的证据[J]. 心理学报, 2017, 49(7): 928-940. |
| [12] | 周宵;伍新春;曾旻;田雨馨. 青少年的情绪调节策略对创伤后应激障碍和创伤后成长的影响:社会支持的调节作用[J]. 心理学报, 2016, 48(8): 969-980. |
| [13] | 任志洪; 李献云; 赵陵波; 余香莲; 李政汉; 赖丽足; 阮怡君; 江光荣. 抑郁症网络化自助干预的效果及作用机制 ——以汉化MoodGYM为例[J]. 心理学报, 2016, 48(7): 818-832. |
| [14] | 白学军;岳鹏飞. 情绪标注对负性情绪的抑制:来自自主神经活动的证据[J]. 心理学报, 2013, 45(7): 715-724. |
| [15] | 唐淦琦,黄敏儿. 高低幸福感人群的负情绪特点:生理和表情的依据[J]. 心理学报, 2012, 44(8): 1086-1099. |
PDF全文下载地址:
http://journal.psych.ac.cn/xlxb/CN/article/downloadArticleFile.do?attachType=PDF&id=4932
