 ), 王宴庆2,3, 李晴1, 许珍珍1, 龙泉杉1
), 王宴庆2,3, 李晴1, 许珍珍1, 龙泉杉1 1 西南大学心理学部, 认知与人格教育部重点实验室, 重庆 400715
2 中国科学院心理研究所, 北京 100101
3 中国科学院大学心理学系, 北京 100049
收稿日期:2019-01-14出版日期:2020-02-25发布日期:2019-12-24通讯作者:陈安涛E-mail:xscat@swu.edu.cn基金资助:* 国家自然科学基金项目(61431013);国家自然科学基金项目(31771254);中央高校基本科研业务费专项资金(SWU1609106);中央高校基本科研业务费专项资金(SWU1709107);中央高校基本科研业务费专项资金(SWU1809361)Acute stress impairs error monitoring and post-error adjustment
HU Na1, CHEN Antao1( ), WANG Yanqing2,3, LI Qing1, XU Zhenzhen1, LONG Quanshan1
), WANG Yanqing2,3, LI Qing1, XU Zhenzhen1, LONG Quanshan1 1 Key Laboratory of Cognition and Personality of Ministry of Education, Faculty of Psychology, Southwest University, Chongqing 400715, China
2 Institute of Psychology, Chinese Academy of Sciences, Beijing 100101, China
3 Department of Psychology, University of Chinese Academy of Sciences, Beijing 100049, China
Received:2019-01-14Online:2020-02-25Published:2019-12-24Contact:CHEN Antao E-mail:xscat@swu.edu.cn摘要/Abstract
摘要: 生活中, 个体会时时关注自己的行为结果并及时做出调整以适应环境的变化。但在应激下个体能否有效地监控行为并做出适应性调整依然未知。本研究招募了52名男性大学生被试, 将其随机分入应激组与控制组, 采用特里尔社会应激测试(Trier Social Stress Test, TSST)诱发个体的应激反应, 并结合错误意识任务(Error Awareness Task, EAT)探索个体急性应激下的错误监控与错误后调整过程。应激指标的结果显示应激组个体在应激任务后唾液皮质醇、心率、应激感知自我报告和负性情绪均显著高于控制组, 表明急性应激的诱发是成功的。行为结果显示应激组的错误意识正确率显著低于控制组, 错误意识反应时显著短于控制组; 进一步地, 应激组个体在意识到错误之后的试次上正确率显著低于未意识到错误之后的试次, 并且应激组个体在意识到错误之后的试次上正确率低于控制组。结果表明急性应激降低了个体对错误反应的监控水平, 即便在辨别出错误反应的情况下, 个体的行为监控与调节也更差。本研究说明急性应激会损伤行为监控系统, 导致个体的行为适应性下降。
图/表 7
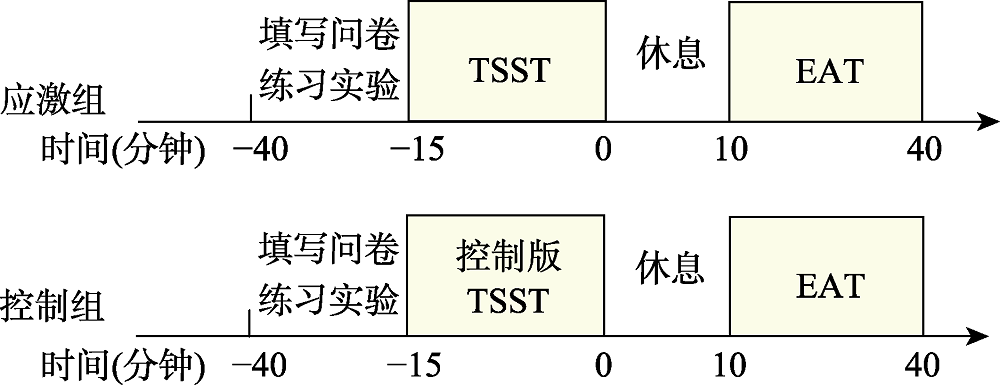
图1实验流程
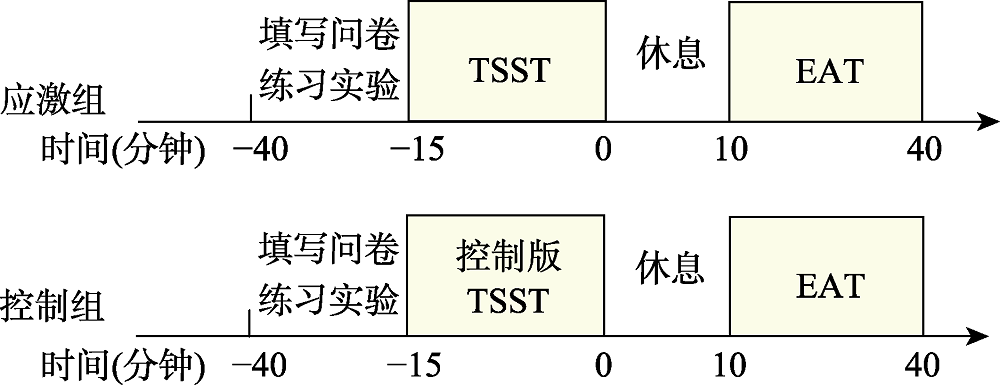 图1实验流程
图1实验流程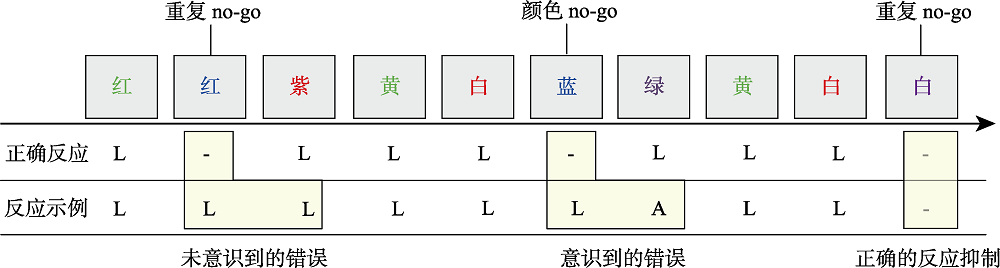
图2错误意识任务流程图
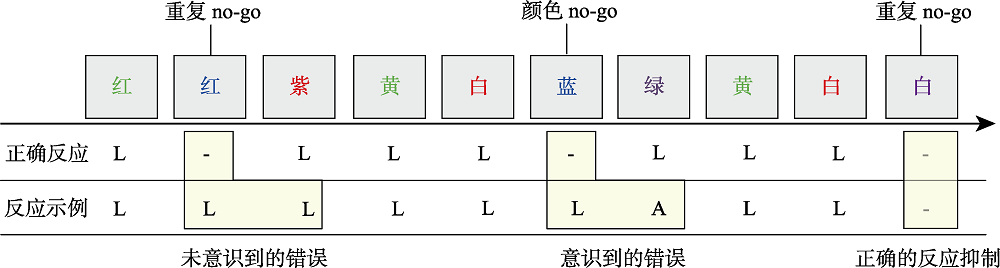 图2错误意识任务流程图
图2错误意识任务流程图
图3应激的生理测量和主观报告 注:* p < 0.05, *** p < 0.001
 图3应激的生理测量和主观报告 注:* p < 0.05, *** p < 0.001
图3应激的生理测量和主观报告 注:* p < 0.05, *** p < 0.001表1go和no-go试次的正确率和反应时
| 类别 | 试次类型 | 应激组 | 控制组 | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| 正确率(%) | go | 95.85 | 6.18 | 96.96 | 2.43 |
| 颜色no-go | 28.42 | 20.48 | 40.64 | 14.97 | |
| 重复no-go | 45.04 | 21.66 | 61.41 | 18.22 | |
| 反应时(ms) | go | 453.30 | 87.86 | 492.35 | 57.41 |
| 颜色no-go | 450.77 | 95.53 | 500.38 | 53.26 | |
| 重复no-go | 468.71 | 111.38 | 511.33 | 84.13 | |
表1go和no-go试次的正确率和反应时
| 类别 | 试次类型 | 应激组 | 控制组 | ||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| 正确率(%) | go | 95.85 | 6.18 | 96.96 | 2.43 |
| 颜色no-go | 28.42 | 20.48 | 40.64 | 14.97 | |
| 重复no-go | 45.04 | 21.66 | 61.41 | 18.22 | |
| 反应时(ms) | go | 453.30 | 87.86 | 492.35 | 57.41 |
| 颜色no-go | 450.77 | 95.53 | 500.38 | 53.26 | |
| 重复no-go | 468.71 | 111.38 | 511.33 | 84.13 | |

图4错误意识任务的反应时与正确率 注:* p < 0.05, *** p < 0.001
 图4错误意识任务的反应时与正确率 注:* p < 0.05, *** p < 0.001
图4错误意识任务的反应时与正确率 注:* p < 0.05, *** p < 0.001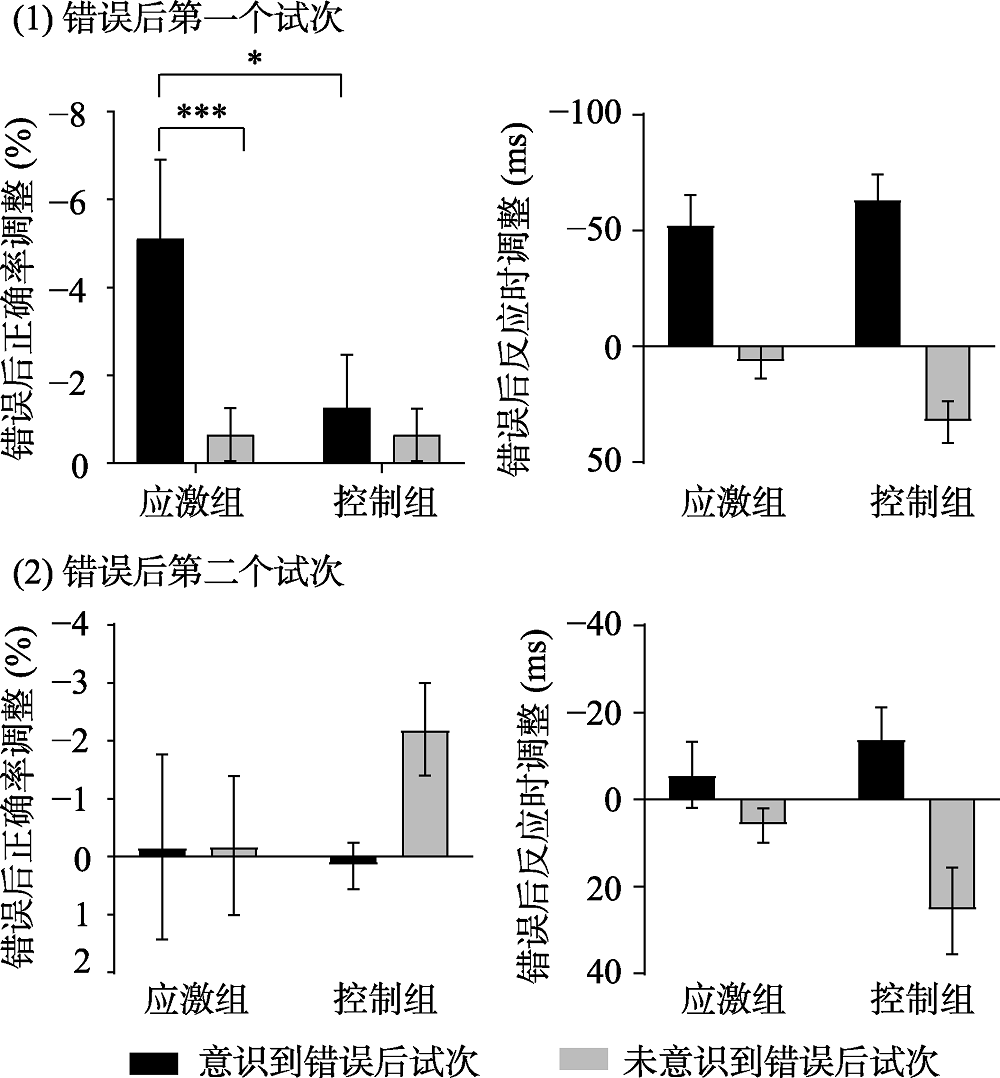
图5错误后调整的正确率与反应时 注:* p < 0.05, *** p < 0.001
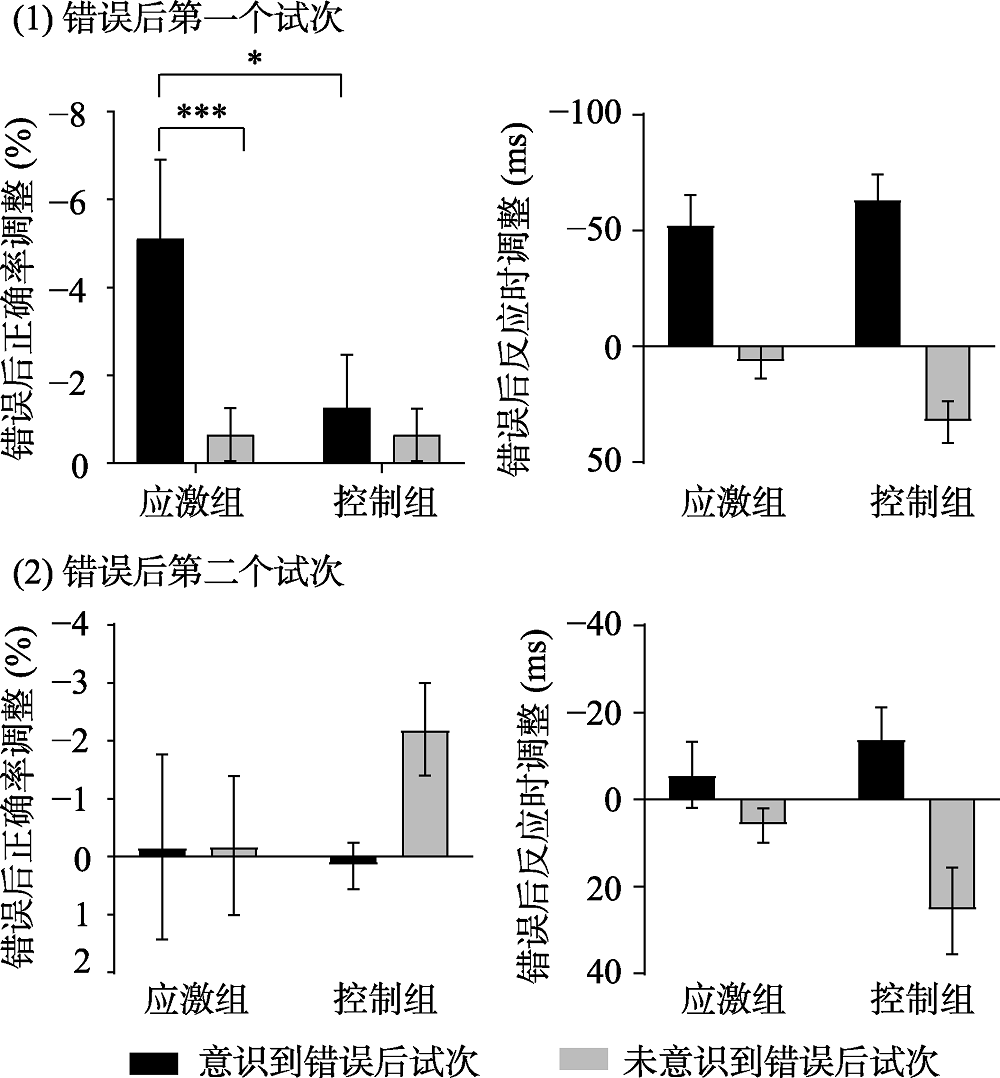 图5错误后调整的正确率与反应时 注:* p < 0.05, *** p < 0.001
图5错误后调整的正确率与反应时 注:* p < 0.05, *** p < 0.001表2错误意识正确率与应激指标的相关分析结果
| 组别 | 值 | 皮质醇 | 心率 | 应激感知自我报告 | 负性情绪 | ||||
|---|---|---|---|---|---|---|---|---|---|
| (t = 0) | (t = 10) | (t = 0) | (t = 10) | (t = 0) | (t = 10) | (t = 0) | (t = 10) | ||
| 控制组 | r | 0.18 | 0.36 | -0.18 | -0.28 | 0.13 | -0.06 | -0.19 | -0.20 |
| p | 0.378 | 0.075 | 0.368 | 0.170 | 0.528 | 0.788 | 0.347 | 0.327 | |
| 应激组 | r | 0.38 | 0.08 | 0.05 | 0.05 | -0.12 | 0.29 | -0.42* | -0.14 |
| p | 0.059 | 0.708 | 0.799 | 0.822 | 0.545 | 0.149 | 0.034 | 0.488 | |
表2错误意识正确率与应激指标的相关分析结果
| 组别 | 值 | 皮质醇 | 心率 | 应激感知自我报告 | 负性情绪 | ||||
|---|---|---|---|---|---|---|---|---|---|
| (t = 0) | (t = 10) | (t = 0) | (t = 10) | (t = 0) | (t = 10) | (t = 0) | (t = 10) | ||
| 控制组 | r | 0.18 | 0.36 | -0.18 | -0.28 | 0.13 | -0.06 | -0.19 | -0.20 |
| p | 0.378 | 0.075 | 0.368 | 0.170 | 0.528 | 0.788 | 0.347 | 0.327 | |
| 应激组 | r | 0.38 | 0.08 | 0.05 | 0.05 | -0.12 | 0.29 | -0.42* | -0.14 |
| p | 0.059 | 0.708 | 0.799 | 0.822 | 0.545 | 0.149 | 0.034 | 0.488 | |
参考文献 45
| [1] | Arnsten A. F . (2015). Stress weakens prefrontal networks: Molecular insults to higher cognition. Nature Neuroscience, 18(10), 1376-1385. |
| [2] | Banich M. T . (2009). Executive function: The search for an integrated account. Current Directions in Psychological Science, 18(2), 89-94. |
| [3] | Beck A. T . (1968). Depression: Clinical, experimental and theoretical aspects. JAMA, 203(13), 1144-1145. |
| [4] | Bogdanov M., & Schwabe L . (2016). Transcranial stimulation of the dorsolateral prefrontal cortex prevents stress-induced working memory deficits. Journal of Neuroscience, 36(4), 1429-1437. |
| [5] | Botvinick M. M., Braver T. S., Barch D. M., Carter C. S., & Cohen J. D . (2001). Conflict monitoring and cognitive control. Psychological Review, 108(3), 624-652. |
| [6] | Buzzell G. A., Beatty P. J., Paquette N. A., Roberts D. M., & McDonald C. G . (2017). Error-induced blindness: Error detection leads to impaired sensory processing and lower accuracy at short response-stimulus intervals. The Journal of Neuroscience, 37(11), 2895-2903. |
| [7] | Cavanagh J. F., & Allen J. J . (2008). Multiple aspects of the stress response under social evaluative threat: An electrophysiological investigation. Psychoneuroendocrinology, 33(1), 41-53. |
| [8] | Clemans Z. A., Elbaz A. S., Hollifield M., & Sokhadze E. M . (2012). Single trial time-frequency domain analysis of error processing in post-traumatic stress disorder. Neuroscience Letters, 525(2), 105-110. |
| [9] | Danielmeier C., & Ullsperger M . (2011). Post-error adjustments. Frontiers in Psychology, 2(233), 233. |
| [10] | Dedovic K., Rexroth M., Wolff E., Duchesne A., Scherling C., Beaudry T., ... Pruessner J. C . (2009). Neural correlates of processing stressful information: An event-related fMRI study. Brain Research, 1293(1293), 49-60. |
| [11] | Di Gregorio F., Steinhauser M., & Maier M. E . (2016). Error-related brain activity and error awareness in an error classification paradigm. NeuroImage, 139, 202-210. |
| [12] | Dickerson S. S., Gruenewald T. L., & Kemeny M. E . (2004). When the social self is threatened: Shame, physiology, and health. Journal of Personality, 72(6), 1191-1216. |
| [13] | Dutilh G., Ravenzwaaij D. V., Nieuwenhuis S., Han L. J. V. D., Forstmann B. U., & Wagenmakers E. J . (2012). How to measure post-error slowing: A confound and a simple solution. Journal of Mathematical Psychology, 56(3), 208-216. |
| [14] | Endrass T., Reuter B., & Kathmann N . (2007). ERP correlates of conscious error recognition: Aware and unaware errors in an antisaccade task. European Journal of Neuroscience, 26(6), 1714-1720. |
| [15] | Falconer E., Bryant R., Felmingham K. L., Kemp A. H., Gordon E., Peduto A., ... Williams L. M . (2008). The neural networks of inhibitory control in posttraumatic stress disorder. Journal of Psychiatry & Neuroscience, 33(5), 413-422. |
| [16] | Fumi K., & Christos C . (2012). Early involvement of prefrontal cortex in visual bottom-up attention. Nature Neuroscience, 15(8), 1160-1166. |
| [17] | Gehring W. J., Goss B., Coles M., Meyer D. E., & Donchin E . (2018). The error-related negativity. Perspectives on Psychological Science, 13(2), 200-204. |
| [18] | Hajcak G., & Dan F . (2008). Errors are aversive: Defensive motivation and the error-related negativity. Psychological Science, 19(2), 103-108. |
| [19] | Hermans E. J., Henckens M. J., Joëls M., & Fernández G . (2014). Dynamic adaptation of large-scale brain networks in response to acute stressors. Trends in neurosciences, 37(6), 304-314. |
| [20] | Hester R., Foxe J. J., Molholm S., Shpaner M., & Garavan H . (2005). Neural mechanisms involved in error processing: A comparison of errors made with and without awareness. Neuroimage, 27(3), 602-608. |
| [21] | Hester R., Simoes-Franklin C., & Garavan H . (2007). Post-error behavior in active cocaine users: Poor awareness of errors in the presence of intact performance adjustments. Neuropsychopharmacology, 32(9), 1974-1978. |
| [22] | Hester R., Nandam L. S., O'Connell R. G., Wagner J., Strudwick M., Nathan P. J., ... Nandam L. S . (2012). Neurochemical enhancement of conscious error awareness. Journal of Neuroscience, 32(8), 2619-2627. |
| [23] | Inzlicht M., Bartholow B. D., & Hirsh J. B . (2015). Emotional foundations of cognitive control. Trends in cognitive sciences, 19(3), 126-132. |
| [24] | Jentzsch I., & Dudschig C . (2009). Why do we slow down after an error? Mechanisms underlying the effects of posterror slowing. The Quarterly Journal of Experimental Psychology, 62(2), 209-218. |
| [25] | Kirschbaum C., Kudielka B. M., Gaab J., Schommer N. C., & Hellhammer D. H . (1999). Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosomatic Medicine, 61(2), 154-162. |
| [26] | Laming D . (1979). Choice reaction performance following an error. Acta Psychologica, 43(3), 199-224. |
| [27] | Laredo S. A., Steinman M. Q., Robles C. F., Ferrer E., Ragen B. J., ... Trainor B. C . (2015). Effects of defeat stress on behavioral flexibility in males and females: Modulation by the mu-opioid receptor. European Journal of Neuroscience, 41(4), 434-441. |
| [28] | Luu P., Collins P., & Tucker D. M . (2000). Mood, personality, and self-monitoring: Negative affect and emotionality in relation to frontal lobe mechanisms of error monitoring. Journal of Experimental Psychology General, 129(1), 43-60. |
| [29] | McReynolds J. R., Donowho K., Abdi A., McGaugh J. L., Roozendaal B., & McIntyre C. K . (2010). Memory- enhancing corticosterone treatment increases amygdala norepinephrine and arc protein expression in hippocampal synaptic fractions. Neurobiology of learning and memory, 93(3), 312-321. |
| [30] | Pessoa L . (2009). How do emotion and motivation direct executive control? Trends in Cognitive Sciences, 13(4), 160-166. |
| [31] | Plessow F., Fischer R., Kirschbaum C., & Goschke T . (2011). Inflexibly focused under stress: Acute psychosocial stress increases shielding of action goals at the expense of reduced cognitive flexibility with increasing time lag to the stressor. Journal of Cognitive Neuroscience, 23(11), 3218-3227. |
| [32] | Pruessner J. C., Dedovic K., Khalili-Mahani N., Engert V., Pruessner M., Buss C., ... Lupien S . (2008). Deactivation of the limbic system during acute psychosocial stress: Evidence from positron emission tomography and functional magnetic resonance imaging studies. Biological Psychiatry, 63(2), 234-240. |
| [33] | Qin S., Hermans E. J., van Marle H. J. F., Luo J., & Fernández G . (2009). Acute psychological stress reduces working memory-related activity in the dorsolateral prefrontal cortex. Biological Psychiatry, 66(1), 25-32. |
| [34] | Roozendaal B., Okuda S., van der Zee E. A., & McGaugh J. L . (2006). Glucocorticoid enhancement of memory requires arousal-induced noradrenergic activation in the basolateral amygdala. Proceedings of the National Academy of Sciences, 103(17), 6741-6746. |
| [35] | Sänger J., Bechtold L., Schoofs D., Blaszkewicz M., & Wascher E . (2014). The influence of acute stress on attention mechanisms and its electrophysiological correlates. Frontiers in Behavioral Neuroscience, 8, 353. |
| [36] | Spielberger C. D . (1989). State-Trait Anxiety Inventory: A comprehensive bibliography. Consulting Psychologists Press |
| [37] | Steinhauser M., Ernst B., & Ibald K. W . (2017). Isolating component processes of posterror slowing with the psychological refractory period paradigm. Journal of Experimental Psychology: Learning, Memory, and Cognition, 43(4), 653-659 |
| [38] | Ullsperger M., & Danielmeier C . (2016). Reducing speed and sight: How adaptive is post-error slowing? Neuron, 89(3), 430-432. |
| [39] | Watson D., Clark L. A., & Tellegen A . (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063-1070. |
| [40] | Weinberg A., Riesel A., & Hajcak G . (2012). Integrating multiple perspectives on error-related brain activity: The ERN as a neural indicator of trait defensive reactivity. Motivation & Emotion, 36(1), 84-100. |
| [41] | Whitton A. E., Veer A. V. T., Kakani P., Dillon D. G., Ironside M. L., Haile A., ... Pizzagalli D. A . (2017). Acute stress impairs frontocingulate activation during error monitoring in remitted depression. Psychoneuroendocrinology, 75, 164-172. |
| [42] | Wu J., Ge Y., Shi Z., Duan X., Wang L., Sun X., ... Zhang K . (2010). Response inhibition in adolescent earthquake survivors with and without posttraumatic stress disorder: A combined behavioral and ERP study. Neuroscience Letters, 486(3), 117-121. |
| [43] | Wu J., Yuan Y., Duan H., Qin S., Buchanan T. W., Zhang K., ... Liang Z . (2014). Long-term academic stress increases the late component of error processing: An ERP study. Biological psychology, 99, 77-82. |
| [44] | Vijayraghavan S., Wang M., Birnbaum S. G., Williams G. V., & Arnsten A. F . (2007). Inverted-U dopamine D1 receptor actions on prefrontal neurons engaged in working memory. Nature Neuroscience, 10(3), 376-384. |
| [45] | Yeung N., Botvinick M. M., & Cohen J. D . (2004). The neural basis of error detection: Conflict monitoring and the error-related negativity. Psychological Review, 111(4), 931-959. |
相关文章 10
| [1] | 李俊娇, 陈伟, 胡琰健, 曹杨婧文, 郑希付. 预期错误与急性应激对不同强度恐惧记忆提取消退的影响[J]. 心理学报, 2021, 53(6): 587-602. |
| [2] | 任志洪, 赵子仪, 余香莲, 赵春晓, 张琳, 林羽中, 张微. 睾酮素与反社会倾向未成年犯的攻击行为:敌意注意偏向的中介和皮质醇的调节作用[J]. 心理学报, 2020, 52(11): 1288-1300. |
| [3] | 王丽君, 索涛, 赵国祥. 未意识到错误影响错误后调整的电生理证据[J]. 心理学报, 2020, 52(10): 1189-1198. |
| [4] | 罗禹, 念靖晴, 鲍未, 张静静, 赵守盈, 潘运, 许爽, 张禹. 急性应激损害对威胁刺激的注意解除[J]. 心理学报, 2020, 52(1): 26-37. |
| [5] | 彭惠妮, 吴健辉, 孙小方, 关青, 罗跃嘉. 特质焦虑对急性心理性应激反应的预测 *[J]. 心理学报, 2018, 50(9): 997-1006. |
| [6] | 陆青云;陶芳标;侯方丽;孙莹. 青少年应激下皮质醇应答与风险决策相关性的性别差异[J]. 心理学报, 2014, 46(5): 647-655. |
| [7] | 贺琼;王争艳;王莉;蒋彩虹;上官芳芳. 新入园幼儿的皮质醇变化与上呼吸道感染的关系:气质的作用[J]. 心理学报, 2014, 46(4): 516-527. |
| [8] | 王丽杰,孙秋德,严进,刘爱丽,董建树,刘佳佳,王建平. 慢性军事应激致军人海马形态、认知功能和应对方式的变化[J]. 心理学报, 2011, 43(07): 792-797. |
| [9] | 杨娟,侯燕,杨瑜,张庆林. 特里尔社会应激测试(TSST)对唾液皮质醇分泌的影响[J]. 心理学报, 2011, 43(04): 403-409. |
| [10] | 李欢欢,林文娟,李俊发. 急性情绪应激对大鼠行为和脑神经颗粒素磷酸化水平的影响[J]. 心理学报, 2006, 38(04): 576-582. |
PDF全文下载地址:
http://journal.psych.ac.cn/xlxb/CN/article/downloadArticleFile.do?attachType=PDF&id=4629
