
 , 刘浏, 黄治华, 赵慧艳
, 刘浏, 黄治华, 赵慧艳 恩施土家族苗族自治州中心医院 西医部 放射科, 湖北 恩施 445000
2019-05-21 收稿, 2019-06-27 录用
*通讯作者: 陈华东, E-mail: 14877391@qq.com
摘要: 本文对产前超声联合核磁共振成像(MRI)筛查胎儿中枢神经系统(CNS)畸形的价值进行了分析。研究对象选取2016年1月~2019年2月本院收治的疑似胎儿CNS畸形的孕妇196例,所有孕妇均给予产前超声、MRI检查,以产后结果为对照,分析产前超声、MRI及二者联合对胎儿CNS畸形的筛查价值。结果显示,产后胎儿CNS畸形84例(42.86%);在筛查胎儿CNS畸形方面,产前超声敏感度、特异度、准确度分别为80.95%(68/84)、76.79%(86/112)、78.57%(154/196),产前MRI分别为88.10%(74/84)、82.14%(92/112)、84.69%(166/196),产前超声联合MRI分别为97.62%(82/84)、94.64%(106/112)、95.92%(188/196),产前超声联合MRI明显优于产前超声、MRI,差异有统计学意义(P < 0.05)。产前超声与MRI比较,差异无统计学意义(P>0.05)。本文证实了产前超声、MRI对胎儿CNS畸形具有良好的筛查价值,且二者联合的筛查价值更高。
关键词: 产前超声核磁共振成像胎儿中枢神经系统畸形筛查价值
The Value of Prenatal Ultrasound Combined with MRI in Screening Fetal Central Nervous System Malformations
XIANG Haibo, CHEN Huadong

 , LIU Liu, HUANG Zhihua, ZHAO Huiyan
, LIU Liu, HUANG Zhihua, ZHAO Huiyan Department of Radiology, Western Medicine Department, The Central Hospital of Enshi Tujia and Miao Autonomous Prefecture, Enshi 445000, Hubei, P. R. China
*Corresponding author: CHEN Huadong, E-mail: 14877391@qq.com
Abstract: The value of prenatal ultrasound combined with magnetic resonance imaging (MRI) in screening fetal central nervous system (CNS) malformations was analyzed in this study. From January 2016 to February 2019, 196 pregnant women suspected of fetal CNS malformation were selected as the subjects of study. All pregnant women were examined by prenatal ultrasound and MRI. The postpartum results showed that 84 cases (42.86%) had CNS malformation. The sensitivity, specificity and accuracy of the prenatal ultrasound in screening fetal CNS deformities were 80.95% (68/84), 76.79% (86/112), 78.57% (154/196), while the prenatal MRI were 88.10% (74/84), 82.14% (92/112), 84.69% (166/196). The sensitivity, specificity and accuracy of the prenatal ultrasound combined with MRI were 97.62% (82/84), 94.64% (106/112), 95.92% (188/196), which were significantly higher than single method, the difference was statistically significant (P < 0.05). And there was no significant difference between prenatal ultrasound and MRI (P>0.05). This study confirms that prenatal ultrasound and MRI have the good screening value for fetal CNS malformation, and the combination of them has the higher screening value.
Key words: prenatalultrasoundmagnetic resonance imagingfetal central nervous system malformationsscreening value
胎儿中枢神经系统(central nervous system, CNS)畸形是常见的出生缺陷之一,且随着二胎政策的开放,高龄二胎孕产妇持续快速增加,其发病率也逐年增高,已成为我国面临的严峻的公共卫生问题[1]。目前,超声检查是胎儿CNS畸形常用的产前筛查方法之一,具有经济、安全、方便等特点,但仍有部分患儿误诊、漏诊,故如何有效提高其诊断效能具有重要的临床意义[2]。
近年来,随着医疗技术的发展与成熟,尤其是核磁共振成像(MRI)快速成像序列的开发和应用,其已逐渐被应用于产前疾病筛查中,且因具有良好的诊断效能而受到关注和重视[3]。对此,本研究通过给予疑似胎儿CNS畸形的孕妇产前超声、MRI检查,并以产后结果为对照,探讨二者单独及联合对胎儿CNS畸形的筛查价值。
1 资料与方法1.1 一般资料本研究经本院伦理委员会审批通过。研究对象选取2016年1月~2019年2月本院收治的疑似胎儿CNS畸形的孕妇196例,纳入标准:①经超声、临床症状、病史、妇科等检查怀疑胎儿CNS畸形; ②年龄20~40岁,无精神病病史; ③单胎、头位妊娠且在本院生产; ④孕妇或其家属签署知情同意书。排除标准:①有超声或MRI检查禁忌症; ②有阴道大出血、急性胎儿宫内窘迫等疾病; ③有心、肝、肾等严重性疾病; ④资料缺失、早期失去随访者。孕妇年龄20~40岁,平均年龄(32.18±6.17)岁;孕24~32周,平均(27.67±3.11)周;体质量指数20.54~30.47 kg/m2,平均(25.03±3.07)kg/m2。
1.2 实验方法所有孕妇均给予产前超声和MRI检查:产前超声检查,采用美国GE Voluson E8 Expert、Voluson 730 Pro V型彩色多普勒超声诊断仪(探头频率2.5~5.0 MHz),孕妇取仰卧位,常规扫查胎儿颅脑侧脑室、丘脑、小脑等平面,必要时行三维超声或阴道超声(探头频率5.0~10.0 MHz);产前MRI检查,采用GE公司Signa HDe 1.5T磁共振扫描仪(2个体线圈),孕妇取仰卧位、头先进,行盆腔定位扫描及胎儿颅脑轴位、矢状位、冠状位扫描,快速自旋回波序列(TR 1350 ms、TE 67 ms、反转角70°、矩阵256×256、扫描时间22 s、层厚4 mm、间隔30%),真稳态进动快速成像序列(TR 3.91 ms、TE 1.96 ms、反转角45°、矩阵256×256、扫描时间11 s、层厚4 mm),T1WI采用超快速小角度激发序列(TR 169 ms、TE 4.76 ms、反转角70°、扫描时间34 s、层厚4 mm)。弥散加权成像选用b值(50 s/mm2、400 s/mm2、800 s/mm2),一次扫描完成并自动生成ADC图。
1.3 观察指标和标准所有怀疑胎儿CNS畸形的孕妇均由2名副高级职称以上影像科医师采取双盲法阅片,如有意见不一致时则共同讨论最终得出影像学诊断结论,随访并以产后结果为对照,统计分析所有孕妇的产前超声、MRI及产后结果情况,其中胎儿CNS畸形包括侧脑室扩张、后颅窝池、透明隔腔变异、前脑无裂、脑内肿瘤、Dandy-Walker畸形、颅内囊肿、小头畸形等,符合产前超声或MRI诊断即为产前超声联合MRI诊断。敏感度、特异度、准确度采用四格表法计算,敏感度=真畸形数/畸形数,特异度=真无畸形数/无畸形数,准确度=(真畸形数+真无畸形数)/总数[4, 5]。
1.4 统计学分析采用SPSS 22.0软件,计数资料以(%)表示,采用χ2检验,计量资料以(x±s)表示,采用t检验,P < 0.05认为有统计学差异。
2 结果2.1 疑似胎儿CNS畸形孕妇的产前超声、MRI及产后结果本研究产后结果显示,196例疑似胎儿CNS畸形的孕妇中,胎儿CNS畸形84例(42.86%),其中侧脑室扩张28例、后颅窝池22例、透明隔腔变异10例、前脑无裂4例、脑内肿瘤2例、Dandy-Walker畸形8例、颅内囊肿8例、小头畸形2例。胎儿CNS畸形孕妇的产前超声、MRI及产后结果,见表 1。典型病例见图 1。
表1
| 表 1 胎儿CNS畸形孕妇的产前超声、MRI及产后结果(n) Prenatal ultrasound, MRI and postpartum results of pregnant women with CNS malformation (n) |
图 1
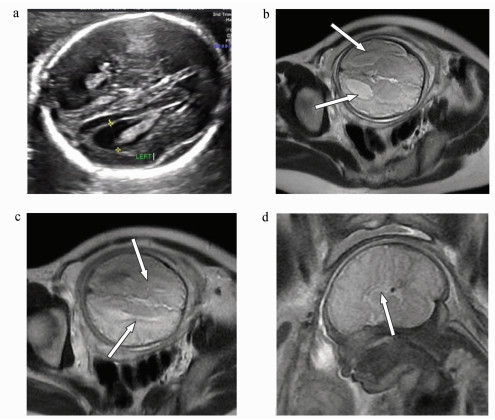 | 图 1 胎儿CNS畸形产前超声及MRI图像:女,孕34周,产后结果显示脑胼胝体发育不良(胼胝体部分缺如) a.产前超声,示胎儿颅脑双侧侧脑室后角扩张,双侧侧脑室体部分离,透明隔间腔未见显示;b、c.产前MRI(T2WI水平位),示胎儿颅脑双侧侧脑室前角分离,体部距离增宽,三角区和后角扩大,呈“蝙蝠翼”状,第三脑室扩大并向前上移位;d.产前MRI(T2WI矢状位),示胎儿颅脑胼胝体膝部及部分体部显示,体积较小,其体部后半部分及压部未见显示 Prenatal ultrasound and MRI images of fetal CNS malformations: female, 34 weeks gestation, postpartum results show dysplasia of the corpus callosum (absence of corpus callosum) a. Prenatal ultrasound showed bilateral ventricular posterior horn dilatation, bilateral ventricular body partially detached, and transparent septal cavity was not shown; b, c. prenatal MRI (T2WI horizontal position) showed that the anterior horn of bilateral ventricles of the fetal brain was separated, the body distance was widened, the triangle area and posterior horn were enlarged, showing a "bat wing" shape, and the third ventricle was enlarged and displaced upward; d. prenatal magnetic resonance imaging (T2WI sagittal) showed that the knee and part of the body of the fetal corpus callosum were small in size, but the posterior part and the pressure part of the body were not shown |
2.2 不同方法筛查胎儿CNS畸形的效能分析在筛查胎儿CNS畸形时,产前超声敏感度、特异度、准确度分别为80.95%(68/84)、76.79%(86/112)、78.57%(154/196),产前MRI分别为88.10%(74/84)、82.14%(92/112)、84.69%(166/196),产前超声联合MRI分别为97.62%(82/84)、94.64%(106/112)、95.92%(188/196),见表 2。
表2
| 表 2 不同方法筛查胎儿CNS畸形的效能分析(n) Effectiveness analysis of different methods for screening CNS malformation of fetuses (n) | ||||||||||||||||||||||||||||||||||
2.3 不同方法筛查胎儿CNS畸形的效能比较在筛查胎儿CNS畸形敏感度、特异度、准确度方面,产前超声联合MRI明显优于产前超声、MRI,差异有统计学意义(P < 0.05),产前超声与MRI比较,差异无统计学意义(P>0.05),见表 3。
表3
| 表 3 不同方法筛查胎儿CNS畸形的效能比较(%) Comparison of the effectiveness of different methods for screening CNS malformations in fetuses (%) | |||||||||||||||||||||||||||||||||||
3 分析与结论胎儿CNS畸形是胎儿畸形中常见类型之一,其发病率约占全部围产儿的0.13%,也是导致婴幼儿畸形、死亡的一个重要因素,其临床诊治日益受到关注和重视[6, 7]。目前,胎儿CNS畸形尚无特效治疗方法,主要采用病因检查治疗,即通过及早检查诊断并以合理终止妊娠等方式处理,以有效减少CNS畸形的出生几率[8, 9],故如何做好孕妇的产前检查并及时采取积极措施,对实现优生优育具有积极的意义。
目前,产前超声检查是公认最重要的胎儿CNS畸形产前检查方法,通过检测超声波接触子宫胎盘、胎儿等后反射的波幅高低,可显示胎儿及其脑部位置、大小、形态等,可及时发现CNS畸形,其筛查价值已逐渐被临床认可[10, 11];但产前超声检查也存在一定局限性,如易受胎儿颅骨回声衰减、脑部血管神经多、结构复杂及孕妇肥胖、胎动、羊水异常等因素干扰,导致误漏诊的发生[12, 13]。而据相关研究报道,MRI可通过强磁场脉冲激发机体目标组织水分子中的氢原子后产生磁共振信息,且具有横断面、冠状面、矢状面等多参数成像的特点,可有效清晰显示病变部位、形态、大小等,近年来已逐渐被应用于胎儿CNS畸形筛查中,且具有良好的筛查效能[14, 15]。但也有研究表明,MRI虽可通过磁共振信息、多参数成像等技术有效显示胎儿脑部及其与周边组织情况,但其费用较为昂贵,且不可清晰显示血流信息,无法实时、动态成像等,易对筛查准确性造成一定影响[15, 16]。
本研究的产后结果显示,胎儿CNS畸形84例(42.86%),产前超声筛查胎儿CNS畸形的敏感度、特异度、准确度分别为80.95%、76.79%、78.57%,产前MRI分别为88.10%、82.14%、84.69%,产前超声与MRI比较无统计学差异,表明产前超声、MRI对胎儿CNS畸形均具有良好的筛查价值,此结论与曾浩、Pfeifer等[12, 13]研究基本相似。这可能是由于产前超声能够通过超声波有效清晰显示胎儿及其脑部位置、大小、形态等,MRI则能够通过强磁场脉冲激发的磁共振信息及多参数成像而有效清晰显示胎儿及其脑部位置、大小、形态等,二者均能够为胎儿CNS畸形提供重要的图像信息,从而起良好的筛查作用。此外,本研究中产前超声联合MRI筛查胎儿CNS畸形的敏感度、特异度、准确度分别为97.62%、94.64%、95.92%,明显高于产前超声和MRI单独使用,表明产前超声、MRI联合对胎儿CNS畸形的筛查价值更高。这可能是由于在单独超声筛查中,易受前述多因素影响,导致部分孕妇未能有效清晰显示胎儿及其脑部位置、大小、形态等,如后颅窝池、透明隔腔变异等畸形易受胎儿体位变化、颅骨影遮挡、孕妇肥胖等影响,从而导致误漏诊的发生。而在单独产前MRI筛查中,可能由于其不可清晰显示血流信息、无法实时动态成像,胎儿及其脑部血管显示不清且不能动态观察其变化,易导致后颅窝池、透明隔腔变异、颅内囊肿等误漏诊的发生,从而影响了筛查准确性。而本研究产前超声和MRI联合筛查时,有效弥补了二者各自的不足,能够为胎儿CNS畸形筛查提供更多、更准确的信息,从而提高了筛查效能。
综上所述,产前超声和MRI对胎儿CNS畸形具有良好的筛查价值,且二者联合的筛查价值更高。
参考文献
| [1] | 华方明, 任苓, 曾庆新, 程玲, 吴牡丹, 叶军. 早孕期胎儿中枢神经系统畸形的超声影像诊断[J]. 中华超声影像学杂志, 2017, 26(5): 410-413. Hua F M, Ren L, Zeng Q X, Cheng L, Wu M D, Ye J. Prenatal ultrasonographic diagnosis of fetal central nervous system abnormalities during the first trimester[J]. Chinese Journal of Ultrasonography, 2017, 26(5): 410-413. DOI:10.3760/cma.j.issn.1004-4477.2017.05.009 |
| [2] | Dall'Asta A, Paramasivam G, Basheer S N, Whitby E, Tahir Z, Lees C. How to obtain diagnostic planes of the fetal central nervous system using three-dimensional ultrasound and a context-preserving rendering technology[J]. American Journal of Obstetrics and Gynecology, 2019, 220(3): 215-229. DOI:10.1016/j.ajog.2018.11.1088 |
| [3] | 张少丹, 陈薇. MRI与常规超声诊断胎儿常见畸形的随机多中心对比分析[J]. 中国CT和MRI杂志, 2015, 13(9): 113-115. Zhang S D, Chen W. Randomized multi-center comparative analysis on MRI and conventional ultrasound in the diagnosis of fetal abnormalityies[J]. Chinese Journal of CT and MRI, 2015, 13(9): 113-115. DOI:10.3969/j.issn.1672-5131.2015.09.035 |
| [4] | 戴琳, 章春泉. 产前超声联合磁共振在胎儿中枢神经系统畸形诊断中的应用价值[J]. 中国当代医药, 2018, 25(19): 135-137. Dai L, Zhang C Q. The value of prenatal ultrasound combined with magnetic resonance in deformity of fetal central nervous system[J]. China Modern Medicine, 2018, 25(19): 135-137. DOI:10.3969/j.issn.1674-4721.2018.19.042 |
| [5] | Shin J E, Shin J C, Kim S J, Lee Y, Im S A, Park I Y. Contribution of magnetic resonance imaging to ultrasound for the evaluation of fetal central nervous system anomalies[J]. Journal of Reproductive Medicine, 2017, 62(5/6): 295-299. |
| [6] | 杨建军, 姜红芳, 耿书军. 三维彩超对胎儿中枢神经系统畸形的诊断应用价值[J]. 医学影像学杂志, 2016, 26(1): 18-21. Yang J J, Jiang H F, Geng S J. The applying values of three-dimensional ultrasound for diagnosis of fetal malformations of the central nervous system[J]. Journal of Medical Imaging, 2016, 26(1): 18-21. |
| [7] | Troisi J, Landolfi A, Sarno L, Richards S, Symes S, Adair D, Ciccone C, Scala G, Martinelli P, Guida M. A metabolomics-based approach for non-invasive screening of fetal central nervous system anomalies[J]. Metabolomics, 2018, 14(6): 77. DOI:10.1007/s11306-018-1370-8 |
| [8] | 鲍天萍, 石德峰, 牛宗保. 超声联合MRI对胎儿中枢神经系统畸形的诊断价值[J]. 中国实用神经疾病杂志, 2016, 19(3): 92-94. Bao T P, Shi D F, Niu Z B. Diagnostic value of ultrasound combined with MRI in fetal central nervous system malformation[J]. Chinese Journal of Practical Neruous Diseases, 2016, 19(3): 92-94. DOI:10.3969/j.issn.1673-5110.2016.03.057 |
| [9] | Engels A C, Joyeux L, Brantner C, De Keersmaecker B, De Catte L, Baud D, Deprest J, Van Mieghem T. Sonographic detection of central nervous system defects in the first trimester of pregnancy[J]. Prenatal Diagnosis, 2016, 36(3): 266-73. DOI:10.1002/pd.4770 |
| [10] | 胡剑, 王相玉, 何媛, 艾清秀, 简雅婷. 超声及MRI诊断胎儿中枢神经系统畸形灵敏度、特异度比较[J]. 现代仪器与医疗, 2016, 22(4): 4-5. Hu J, Wang X Y, He Y, Ai Q X, Jian Y T. Comparison of sensitivity and specificity between ultrasound and MRI in diagnosis of fetal central nervous system malformations[J]. Modern Instruments, 2016, 22(4): 4-5. |
| [11] | Domr?se C M, Bremer S, Buczek C, Geipel A, Berg C, Hellmund A, Gembruch U, Willruth A. Termination of pregnancy following prenatally diagnosed central nervous system malformations[J]. Archives of Gynecology and Obstetrics, 2018, 298(5): 903-910. DOI:10.1007/s00404-018-4900-8 |
| [12] | 曾浩, 彭敏. 产前MRI、US检查对胎儿中枢神经系统畸形的诊断效果比较[J]. 中国实验诊断学, 2018, 22(8): 1299-1302. Zeng H, Peng M. Comparison of prenatal MRI and US examination in the diagnosis of fetal central nervous system malformation[J]. Chinese Journal of Laboratory Diagnosis, 2018, 22(8): 1299-1302. DOI:10.3969/j.issn.1007-4287.2018.08.001 |
| [13] | Pfeifer C M. Maternal-fetal medicine specialists should manage patients requiring fetal MRI of the central nervous system[J]. AJNR American Journal of Neuroradiology, 2019, 40(2): E6. DOI:10.3174/ajnr.A5894 |
| [14] | 陈艺菲. 磁共振成像诊断产前先天性畸形的临床效果[J]. 中国妇幼保健, 2017, 32(8): 1791-1793. Cheng Y F. Clinical effect of magnetic resonance imaging in diagnosis of prenatal congenital malformations[J]. Maternal and Child Health Care of China, 2017, 32(8): 1791-1793. |
| [15] | Irwin K, Henry A, Gopikrishna S, Taylor J, Welsh A W. Utility of fetal MRI for workup of fetal central nervous system anomalies in an Australian maternal-fetal medicine cohort[J]. Australian and New Zealand Journal of Obstetrics and Gynaecology, 2016, 56(3): 267-73. DOI:10.1111/ajo.12440 |
| [16] | 陶斯翠, 李建蓉, 梁辉, 何雪花, 周杰, 李晶晶, 吴强. 超声与MRI在疑似高危胎儿中枢神经系统异常筛查中应用研究[J]. 中国CT和MRI杂志, 2017, 15(4): 14-16. Tao S C, Li J R, Liang H, He X H, Zhou J, Li J J, Wu Q. Application of ultrasound and MRI in screening of suspected high-risk fetal central nervous system abnormalities[J]. Chinese Journal of CT and MRI, 2017, 15(4): 14-16. DOI:10.3969/j.issn.1672-5131.2017.04.005 |
