
 , 李曦, 谢芳
, 李曦, 谢芳 绵阳市中医医院 超声医学科, 四川 绵阳 621000
2019-06-11 收稿, 2019-07-06 录用
*通讯作者: 胡良勇, E-mail: huliangyongh@126.com
摘要: 本文对超声弹性成像(UE)联合乳腺影像报告和数据系统(BI-RADS)对微小(≤2 cm)乳腺良恶性病变的鉴别价值进行了分析。研究对象选取2018年3月~2019年3月期间本院80例乳腺病变患者共112个病灶,所有患者均给予UE和BI-RADS检查,以病理检查为参照,分析UE、BI-RADS及二者联合对微小(≤2 cm)乳腺良恶性病变的鉴别价值。病理检查结果显示,112个病灶中,良性60个(53.57%)、恶性52个(46.43%);恶性乳腺病变患者UE和BI-RADS评分明显高于良性患者,差异有统计学意义(P < 0.05)。UE鉴别微小乳腺良恶性病变(≤2 cm)的敏感度为76.92%、特异度为76.67%、准确度为76.79%,BI-RADS的敏感度为80.77%、特异度为80.00%、准确度为80.36%,UE联合BI-RADS的敏感度、特异度、准确度分别为96.15%、95.00%、95.54%,可见UE联合BI-RADS的鉴别效果明显优异,差异有统计学意义(P < 0.05)。本文证实了UE、BI-RADS对微小(≤2 cm)乳腺良恶性病变具有良好的鉴别价值,且二者联合的鉴别价值更高。
关键词: 超声弹性成像乳腺影像报告和数据系统微小乳腺良恶性病变(≤2 cm)鉴别价值
The Differential Value of Ultrasound Elastography Combined with BI-RADS in Benign and Malignant Breast Lesions with Small Size (≤2 cm)
HU Liangyong

 , LI Xi, XIE Fang
, LI Xi, XIE Fang Department of Ultrasonic Medicine, Mianyang City Hospital of Traditional Chinese Medicine, Mianyang 621000, Sichuan, P. R. China
*Corresponding author: HU Liangyong, E-mail: huliangyongh@126.com
Abstract: The differential value of ultrasound elastography (UE) combined with breast imaging reporting and data system (BI-RADS) in benign and malignant breast lesions with small size (≤ 2 cm) was analyzed in this study. A total of 112 lesions were selected as the subjects of this study from 80 patients with breast lesions in our hospital from March 2018 to March 2019, and all patients were examined by UE and BI-RADS. The differential value of UE, BI-RADS and their combination for benign and malignant breast lesions (≤ 2 cm) was analyzed with pathological examination as a reference. The pathological examination results showed that, among 112 lesions, there were 60 benign (53.57%) and 52 malignant (46.43%). The UE and BI-RADS scores of patients with malignant breast lesions were significantly higher than those of patients with benign breast lesions, the difference was statistically significant (P < 0.05). The sensitivity, specificity and accuracy in differentiating benign and malignant breast lesions, the UE was 76.92%, 76.67% and 76.79%, the BI-RADS was 80.77%, 80.00% and 80.36%, UE combined BI-RADS was 96.15%, 95.00% and 95.54%, UE combined BI-RADS was significantly higher than the single of UE and BI-RADS, the difference was statistically significant (P < 0.05). This study confirms that, UE and BI-RADS have the good value in differentiating benign and malignant breast lesions with small size (≤ 2 cm), and their combination has the higher value in differentiating benign and malignant breast lesions.
Key words: ultrasound elastographybreast imaging reporting and data systembenign and malignant breast lesions with small size (≤ 2 cm)differential value
乳腺病变是临床常见病、多发病,可分为良性和恶性,其治疗关键在于早发现、早治疗,尤其是恶性病变若未及时诊治,常可转移侵袭肝、肾等重要器官,严重危害患者生命安全[1]。目前,乳腺病变最常用的检查方法为超声检查,其中超声弹性成像(UE)、乳腺影像报告和数据系统(BI-RADS)是临床上应用广泛的诊断方式[2, 3];但UE、BI-RADS单独鉴别乳腺良恶性病变仍有局限性,尤其是对微小病灶(≤2 cm)的误漏诊较高,故如何有效提高该病的鉴别准确度,具有重要的临床意义。对此,本研究通过给予微小乳腺病变(≤2 cm)患者UE和BI-RADS及二者联合鉴别诊断,探讨了UE联合BI-RADS对微小乳腺良恶性病变的鉴别价值。
1 资料与方法1.1 研究对象本研究经伦理委员会审批通过,对象选取本院2018年3月~2019年3月期间收治的80例微小乳腺病变患者,共112个病灶。研究对象纳入标准:①手术或穿刺组织病理检查为乳腺良恶性病变[4]; ②女性、单侧患病、病灶直径≤2 cm; ③无胃癌、肝癌等其他癌症; ④签署知情同意书。研究对象排除标准:①妊娠期或哺乳期女性; ②有本次检查禁忌证; ③有心、肝、肾等严重性疾病; ④检查前1个月曾有化疗、放疗、激素、抗炎等治疗史。
1.2 研究方法所有患者均给予UE和/或BI-RADS检查。
BI-RADS检查:采用SuperSonic Imaging公司的AixPlorer-SWE彩色多普勒超声诊断仪,探头频率4~15 MHz,患者取侧卧位、充分暴露乳房及腋下区等准备,以乳头为中心多切面检查乳房各象限及腋下淋巴结,发现病变时记录距乳头、皮肤及胸大肌距离及位置、形态、大小、边缘、内部回声、血流情况,常规保存图像。
UE检查:BI-RADS检查后选择感兴趣区取样框(大小为>病灶范围2倍),涂抹适量耦合剂。待病变清晰显示,嘱患者屏气后,设置参数为UE模式、弹性测量量程0~180 kPa,调整图像清晰程度(压力与压放频率的综合指标控制在3~4),选择符合标准图像(正常乳腺组织为绿色,脂肪组织为红色),不施压静置3 s,图像稳定后定帧、存储。
1.3 指标观察由同一组具有丰富检查经验(从事该领域3年以上且取得相关专业证书或资格证明)医护人员独立双盲下阅片,以病理检查结果为对照,分析UE、BI-RADS及二者联合对微小乳腺良恶性病变(≤2 cm)的鉴别价值。敏感度=真恶性数/恶性数,特异度=真良性数/良性数,准确度=(真恶性数+真良性数)/总数。
UE标准[4]:病灶绿色占比>90%为1分,病灶中心呈蓝色和周边为绿色为2分,病灶范围内绿色和蓝色占比相近为3分,病灶整体为蓝色或内部有少量绿色为4分,病灶及周边为蓝色、内部有或无绿色为5分。1~3分为良性,4~5分为恶性。
BI-RADS标准[5]:可能良性病变、无可疑恶性病变为1分,良性病变可能性大、低度可疑恶性为2分,良性病变、中度可疑恶性、需短期随访复查为3分,可疑恶性病变、2% < 恶性率≤95%为4分,高度恶性病变、恶性率>95%为5分,组织活检恶性病变为6分,1~3分为良性、4~6分为恶性。
UE联合BI-RADS标准:符合UE或BI-RADS恶性病变诊断为恶性,其余为良性。
1.4 统计学分析采用SPSS 22.0软件,计数资料以(%)表示,采用χ2检验;计量资料以(x±s)表示,采用独立样本t检验,P < 0.05为有统计学差异。
2 结果2.1 乳腺良恶性病变患者病理检查及一般资料病理检查显示,80例乳腺病变患者的112个病灶中,良性44例共60个病灶(53.57%),包括乳腺纤维腺瘤38个、乳腺腺病10个、导管内乳头状瘤6个、乳腺脓肿4例、乳腺炎2个;恶性36例共52个病灶(46.43%),包括浸润性导管癌40个、导管内癌8个、黏液腺癌4个。乳腺良恶性病变患者年龄、体质量指数、患侧、病变直径比较,差异无统计学意义(P>0.05),见表 1。
表1
| 表 1 乳腺良恶性病变患者一般资料比较 Comparison of general data between benign and malignant breast lesions patients |
2.2 乳腺良恶性病变患者UE和BI-RADS评分比较恶性乳腺病变患者UE和BI-RADS评分明显高于良性患者,差异有统计学意义(P < 0.05),见表 2。图 1和图 2是典型病例的UE和BI-RADS图像。
表2
| 表 2 乳腺良恶性病变患者UE和BI-RADS评分比较 Comparison of UE, BI-RADS score between benign and malignant breast lesions patients |
图 1
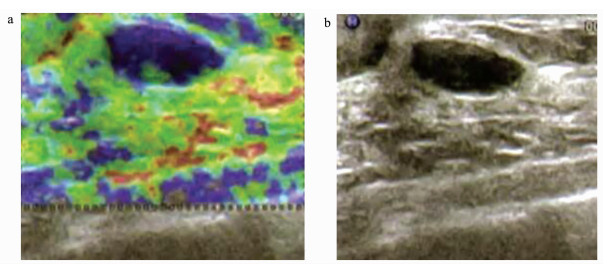 | 图 1 恶性乳腺病变患者UE、BI-RADS图女,42岁,病理检查为浸润性导管癌 UE and BI-RADS in patients with malignant breast lesions Female, 42 years old, pathological examination showed it is invasive ductal carcinoma a. UE; b. BI-RADS |
图 2
 | 图 2 良性乳腺病变患者UE、BI-RADS图女,40岁,病理检查为乳腺炎 UE and BI-RADS in patients with benign breast lesions Female, 40 years old, pathological examination showed it is mastitis a. UE; b. BI-RADS |
2.3 不同方法鉴别微小乳腺良恶性病变(≤2 cm)的价值UE在鉴别微小乳腺良恶性病变(≤2 cm)方面,敏感度为76.92%(40/52),特异度为76.67%(46/60),准确度为76.79%(86/112)。BI-RADS敏感度为80.77%(42/52),特异度为80.00%(48/60),准确度为80.36%(90/112)。UE联合BI-RADS鉴别微小乳腺良恶性病变(≤2 cm)敏感度为96.15%(50/52),特异度为95.00%(57/60),准确度为95.54%(107/112),见表 3。
表3
| 表 3 不同方法鉴别微小乳腺良恶性病变(≤2 cm)的价值 The value of different methods in differentiating benign and malignant breast lesions (≤ 2 cm) | ||||||||||||||||||||||||||||||||||
2.4 不同方法对微小乳腺良恶性病变(≤2 cm)鉴别价值的比较UE联合BI-RADS鉴别微小乳腺良恶性病变(≤2 cm)的敏感度、特异度、准确度,明显高于UE及BI-RADS,差异有统计学意义(P < 0.05),见表 4。
表4
| 表 4 不同方法对微小乳腺良恶性病变(≤2 cm)鉴别价值的比较 Comparison of different methods in differentiating benign and malignant breast lesions (≤2 cm) |
3 讨论乳腺病变是威胁女性身心健康的主要疾病之一,主要表现为单发肿块,可伴发乳头溢液,其中恶性病变即为乳腺癌。因乳腺非人体必要器官,故其原位癌不致命,但随病情进展可转移侵犯肝、肾等而危及患者生命安全[1, 2]。而乳腺癌早期阶段的病变微小(直径≤2 cm),其临床治疗疗效良好、预后佳,但其早期无特异性症状或症状与乳腺良性病变相似,不易被检出,故如何有效鉴别微小(≤2 cm)乳腺良恶性病变具有重要的临床价值[3, 4]。
目前,超声是乳腺病变常用的影像学检查方法,具有简便、安全、无辐射等特点,通过超声波探查目标区域可有效显示组织的形态、大小、边缘、回声、钙化等征象,为临床疾病诊断提供重要的依据[6, 7]。有研究显示,BI-RADS是一种诊断乳腺病变的规范化、标准化影像学方法,可对乳腺超声征象指标进行量化,已被广泛应用于乳腺癌筛查中,其价值已逐渐被认可[8, 9]。但有研究报道,常规超声对脂肪组织丰富的乳腺或小肿块分辨能力较差,玻璃样变、钙化及边界模糊、形状不规则等乳腺恶性病变征象也可表现在部分病情严重的乳腺良性病变中,从而导致BI-RADS的误漏诊[10, 11]。
UE是一种新型超声技术,可通过超声探测对象组织的分子和微观结构而提供组织弹性硬度信息,并以不同色彩编码代表不同组织的硬度,从而为鉴别病变组织的良恶性提供依据[12, 13]。但据相关研究表明,UE在临床诊断中也存在一定的局限性,如相同组织的硬度在一定程度可能会有重叠、患者个体差异等,且组织硬度还受成分比例、排列结构等影响,易导致误漏诊的发生[14, 15]。
本研究结果显示,恶性乳腺病变患者UE和BI-RADS评分明显高于良性患者。UE鉴别微小乳腺良恶性病变(≤2 cm)的敏感度为76.92%、特异度为76.67%、准确度为76.79%,BI-RADS的敏感度为80.77%、特异度为80.00%、准确度为80.36%,表明UE和BI-RADS对微小乳腺良恶性病变(≤2 cm)具有良好的鉴别价值,此结论与柳芊、Gweon等[4, 5]研究相似。这可能是由于在本研究中,通过BI-RADS超声波探查乳腺组织能够有效显示其形态、大小、边缘、内部回声、有无钙化等征象,并能够量化分析上述超声征象指标,有助于及时发现钙化、内部低回声、形态不规则、边界模糊呈蟹足样等乳腺恶性病变征象特征[8, 9],从而对乳腺病变的良恶性作出鉴别诊断。同时,本研究中,通过UE超声探测乳腺组织的分子和微观结构, 可有效显示其组织弹性硬度信息,有助于及时发现质地较硬、弹性较差、显示为蓝色等乳腺恶性病变征象特征[12, 13],从而有效鉴别乳腺病变的良恶性。此外,UE联合BI-RADS鉴别微小乳腺良恶性病变(≤2 cm)的敏感度、特异度、准确度分别为96.15%、95.00%、95.54%,UE联合BI-RADS明显高于UE及BI-RADS,表明二者联合的鉴别价值更高。这可能是由于在单独BI-RADS中,部分病情严重乳腺良性病变会因常规超声对脂肪组织丰富的乳腺或小肿块分辨能力较差而表现为玻璃样变、钙化及边界模糊、形状不规则状等乳腺恶性病变征象;在单独UE中,则可能因部分病情严重乳腺良性病变的组织硬度高,如乳腺纤维腺瘤的组织软硬度取决于腺管和纤维结缔组织的比例和排列构型,病情严重时可引起主导管引流停滞、闭塞而使组织硬度增加,且会受相同组织间的硬度重叠、患者个体差异等影响;因此,UE、BI-RADS单独鉴别时仍具有较大的局限性,而二者联合则可能有效弥补其中存在的不足,提高了对微小(≤2 cm)乳腺良恶性病变的鉴别准确率。
综上所述,UE、BI-RADS对微小乳腺良恶性病变(≤2 cm)具有良好的鉴别价值,且二者联合鉴别的结果更加准确。
参考文献
| [1] | 苏爱江, 罗扬, 毛爱琴. 超声引导下穿刺活检对早期乳腺癌的诊断价值[J]. 实用癌症杂志, 2018, 33(3): 377-379. Su A J, Luo Y, Mao A Q. analysis of diagnostic value of ultrasound-guided core needle biopsy for early breast cancer[J]. The Practical Journal of Cancer, 2018, 33(3): 377-379. DOI:10.3969/j.issn.1001-5930.2018.03.009 |
| [2] | Stepanek T, Constantinou N, Marshall H, Pham R, Thompson C, Dubchuk C, Plecha D. Changes in the utilization of the BI-RADS category 3 assessment in recalled patients before and after the implementation of screening digi-tal breast tomosynthesis[J]. Academic Radiology, 2019. |
| [3] | 周文娟, 陈超, 王林, 王伟伟, 陆月, 刘玲. 剪切波超声弹性成像在鉴别乳腺肿块良恶性中的应用价值[J]. 中国临床研究, 2016, 29(8): 1112-1113. Zhou W J, Chen C, Wang L, Wang W W, Lu Y, Liu L. Application value of shear wave ultrasound elastography in differentiating benign from malignant breast masses[J]. Chinese Medicine of Factory and Mine, 2016, 29(8): 1112-1113. |
| [4] | 柳芊. 超声造影联合弹性成像技术在乳腺疾病诊断上的应用价值[J]. 中国医疗器械信息, 2019, 25(4): 133-134. Liu Q. Application value of contrast-enhanced ultrasound combined with elastography in the diagnosis of breast diseases[J]. China Association for Medical Devices Industry, 2019, 25(4): 133-134. DOI:10.3969/j.issn.1006-6586.2019.04.067 |
| [5] | Gweon H M, Cho N, Kim S Y, Koo H R, Seo M, Chu A, Son E J. Management for BI-RADS category 3 lesions detected in preoperative breast MR imaging of breast cancer patients[J]. European Radiology, 2017, 27(8): 3211-3216. DOI:10.1007/s00330-016-4721-8 |
| [6] | 高军喜, 王颖鑫, 王雅婷, 宋涛. 超声造影特征及定量参数诊断乳腺癌的单因素及多因素分析[J]. 中国超声医学杂志, 2018, 34(6): 488-491. Gao J X, Wang Y X, Wang Y T, Song T. The single factor and multiple factor analysis of the diagnosis of breast cancer with the characteristics and quantitative parameters of contrast-enhanced ultrasound[J]. Chinese Journal of Ultrasound in Medicine, 2018, 34(6): 488-491. DOI:10.3969/j.issn.1002-0101.2018.06.003 |
| [7] | Wang B, Jiang T, Huang M, Wang J, Chu Y H, Zhong L Y, Zheng S S. Evaluation of the response of breast cancer patients to neoadjuvant chemotherapy by combined contrast-enhanced ultrasonography and ultrasound elastography[J]. Experimental and Therapeutic Medicine, 2019, 17(5): 3655-3663. |
| [8] | 张润, 刘双艳, 李伶俐, 姜飞. 乳腺超声造影与彩色多普勒超声在乳腺肿瘤良恶性诊断中应用[J]. 临床军医杂志, 2018, 46(6): 648-649. Zhang R, Liu S Y, Li L L, Jiang F. Application of contrast-enhanced ultrasound and color Doppler ultrasound in the diagnosis of benign and malignant breast tumors[J]. Clinical Journal of Medical Officer, 2018, 46(6): 648-649. |
| [9] | Grimm L J, Zhang J, Baker J A, Soo M S, Johnson K S, Mazurowski M A. Relationships between MRI breast imaging-reporting and data system (BI-RADS) lexicon descriptors and breast cancer molecular subtypes:internal enhancement is associated with luminal B subtype[J]. Breast Journal, 2017, 23(5): 579-582. DOI:10.1111/tbj.12799 |
| [10] | 贺芳, 肖际东, 文欢, 毛玉瑶. S-detect技术辅助超声鉴别诊断最大径≤ 2 cm乳腺良恶性肿块型病灶[J]. 中国医学影像技术, 2018, 34(8): 1207-1210. He F, Xiao J D, Wen H, Mao Y Y. S-detect computer-aided ultrasound in differential diagnosis of benign and malignant mass-like breast lesions with maximum diameter ≤ 2 cm[J]. Chinese Journal of Medical Imaging Technology, 2018, 34(8): 1207-1210. |
| [11] | Zanotel M, Bednarova I, Londero V, Linda A, Lorenzon M, Girometti R, Zuiani C. Automated breast ultrasound:basic principles and emerging clinical applications[J]. Radiologia Medica, 2018, 123(1): 1-12. |
| [12] | 李杰基, 林小影, 程幸, 曹献云. 高频超声及弹性成像技术在非哺乳期乳腺炎的临床应用[J]. 医学影像学杂志, 2016, 26(5): 936-939. Li J J, Lin X Y, Cheng X, Cao X Y. Clinical application of high frequency ultrasound and elastography in non lactation mastitis[J]. Journal of Medical Imaging, 2016, 26(5): 936-939. |
| [13] | Choi H Y, Seo M, Sohn Y M, Kin H R. Shear wave elastography for the diagnosis of small (≤ 2 cm) breast lesions:added value and factors associated with false results[J]. British Journal of Radiology, 2019, 92(1097): 20180341. DOI:10.1259/bjr.20180341 |
| [14] | 谢丽玲, 汤庆, 何玮华, 何炼图. 超声弹性成像面积比对乳腺病灶BI-RADS分级的参考价值分析[J]. 中国妇幼保健, 2015, 30(16): 2677-2679. Xie L L, Tang Q, He W H, He L T. Analysis of reference value of area ratio of ultrasound elastography in BI-RADS classification of breast lesions[J]. Maternal and Child Health Care of China, 2015, 30(16): 2677-2679. |
| [15] | Suvannarerg V, Chitchumnong P, Apiwat W, Lertdamrongdej L, Tretipwanit N, Pisarnturakit P, Psitthinamsuwan P, Thiravit S, Muangsomboon K, Korpraphong P. Diagnostic performance of qualitative and quantitative shear wave elastography in differentiating malignant from benign breast masses, and association with the histological prognostic factors[J]. Quantitative Imaging in Medicine and Surgery, 2019, 9(3): 386-398. |
